Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Herpes zoster (HZ) commonly observed in the elderly and in immune-compromised patients. The prevalence of HZ is 3.6-19.9% in previously reported data. The higher prevalence of HZ in Systemic Lupus Erythematosus (SLE) patients is aggravated by the concomitant use of immunosuppressant and glucocorticoids (GCs). The objective of this study is to determine the prevalence and describe the characteristics of HZ in an SLE cohort.
Methods:
A patient questionnaire was developed to examine HZ in SLE patients. It includes different questions on patient’ demographics, the onset of HZ in relation the SLE onset, pain related to HZ, history of varicella zoster vaccine, anti-viral therapy for HZ, and several estimated risk factors for HZ. The survey was distributed to consecutive SLE patients attending the Lupus Clinic from January 2016 to April 2018. All patients were evaluated according to a standard protocol which includes assessment of disease activity (SLE Disease Activity Index 2000 [SLEDAI-2K]). Analysis included descriptive statistics.
Results:
Of 912 patients who visited the clinic within that period, 412 patients completed the survey. The prevalence of HZ was 127 (30.8%) at a mean age of 47.4 ± 13.7 years. Of these 127 patients, 32 (25.2%) patients experienced recurrent HZ event, occurring within 12.2 ± 12.1 years from the 1st HZ event. The demographic features of SLE patients with and without HZ are presented in Table 1.
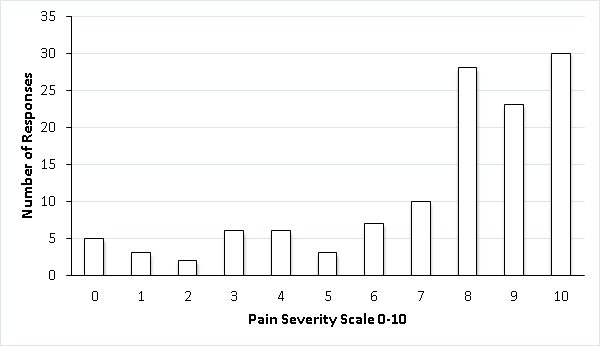
HZ occurred in the first 5 years post SLE diagnosis in 43.1% of patients, 18.1% reported HZ from 6-10 years and 38.2% reported HZ occurrence ≥10 years post SLE diagnosis. Mean SLE duration at first HZ was 9.6 ± 9.8 years. Most (78.8%) of those who developed HZ were not vaccinated prior to HZ. 97.6% of HZ was confirmed by physician and 78% received anti-viral therapy. HZ pain, itching or tingling in the rash area was reported in 96.7% of patients. The majority of the patients reported pain (95.9%) and 74.0% scored between 7-10 (Fig. 1).
Eighty patients (62.9%) reported taking prednisone at the time of HZ. Of those, 32 patients reported a mean prednisone dose of 23.3 mg/day (range, 3–60 mg). Seventy-two patients (56.7%) were on immunosuppressant (Azathioprine 31.5%, Mycophenolate mofetil 14.17%, Methotrexate 6.3% and cyclophosphamide 4.72%).
Conclusion:
The HZ prevalence of 30.8% was higher than previously published data in SLE. HZ can be an early comorbidity in SLE, with 43.1% of cases occurring within 5 years of SLE diagnosis and 57% after 10 years of SLE diagnosis.
Table 1. Demographic characteristic at study visit of patients with and without HZ
|
Characteristic |
Patients who had HZ (N=127) |
Patient who never had HZ (N=285) |
P value |
|
Sex (F) |
118 (92.9%) |
257 (90.2%) |
0.369 |
|
Age in years at SLE diagnosis (mean ± SD) |
30.1 ± 13.1 |
31.0 ± 11.3 |
0.482 |
|
Age in years at study visit (mean ± SD) |
51.9 ± 14.5 |
47.4 ± 13.7 |
0.002 |
|
SLE duration at study visit (mean ± SD) |
21.8 ± 13.2 |
16.3 ± 11.5 |
<0.001 |
|
Ethnicity |
|
|
0.003 |
|
Black |
15 (11.8%) |
62 (21.8%) |
|
|
Caucasian |
86 (67.7%) |
165 (57.9%) |
|
|
Chinese |
17 (13.4%) |
19 (6.7%) |
|
|
Others |
9 (7.1%) |
39 (13.6%) |
|
|
SLE duration at 1st HZ |
9.6 ± 9.8 |
– |
– |
|
Age at first HZ |
47.8 ± 14.1 |
– |
– |
|
Recurrent shingles HZ |
32 (25.2%) |
– |
– |
|
Year from 1stHZ event to 2nd HZ event |
12.2 ± 12.1 |
– |
– |
|
Mean SLEDAI-2K (mean ± SD) |
7.5 ± 7.1 (71/127) |
– |
– |
Figure 1. HZ Pain Severity as Reported by SLE Patients (N=123)
To cite this abstract in AMA style:
Al Rayes H, Anderson N, Bonilla D, Su J, Touma Z. Herpes Zoster in Systemic Lupus Erythematosus: Prevalence and Risk Factors [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/herpes-zoster-in-systemic-lupus-erythematosus-prevalence-and-risk-factors/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/herpes-zoster-in-systemic-lupus-erythematosus-prevalence-and-risk-factors/