Session Information
Date: Monday, November 6, 2017
Title: Health Services Research Poster II: Osteoarthritis and Rheumatoid Arthritis
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior retrospective claims analyses examining rheumatoid arthritis (RA) treatment costs have shown infliximab (IFX) to be costlier than certolizumab pegol (CZP) across all sites of care (physician office, home, outpatient [OP]), primarily due to lower CZP drug costs.1 The present study assessed one-year (yr) healthcare resource utilization (HRU) and costs incurred by RA patients (pts) treated with CZP vs IFX.
Methods: Medical and pharmacy claims data (2008–2015) were derived from the Truven MarketScan® database of insured pts matching the inclusion criteria: RA diagnosis, treatment initiation (index date) with CZP or IFX (July/1/2008–December/31/2014), continuous eligibility ±12 months around index date, and age ≥18 yrs. Mean, unadjusted one-yr visits (OP, inpatient [IP], emergency room [ER], and physician office) and costs (pharmacy, medical, and total healthcare) were calculated and compared between groups via Mann-Whitney U tests. These were also assessed using multivariate (MV) regression models and adjusted for treatment (CZP/IFX), prior biologic use (yes/no), gender, age, baseline health, and baseline HRU and costs.
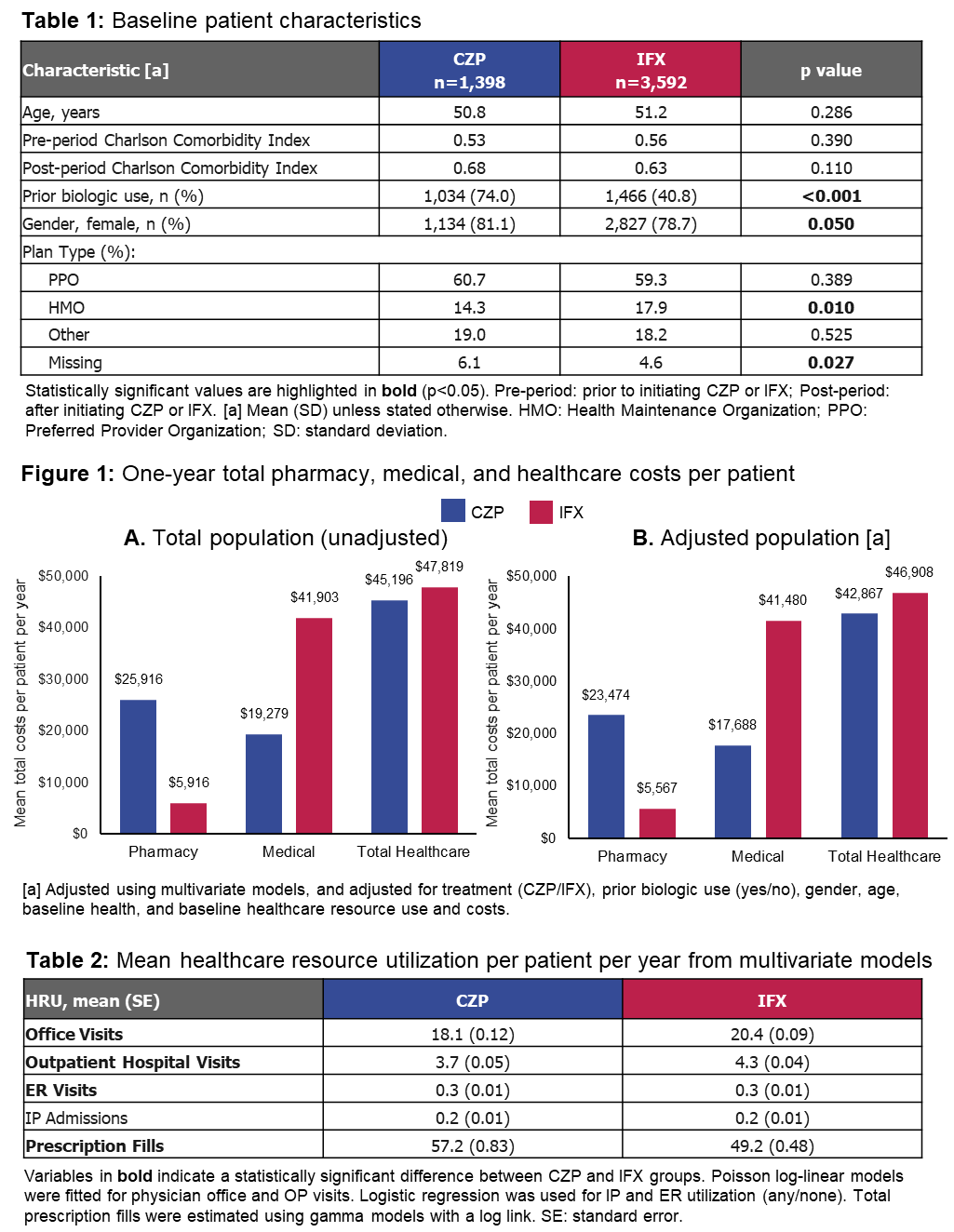
Results: 1,398 RA pts were treated with CZP and 3,592 with IFX. CZP pts were more likely to have prior biologic use than IFX pts (74.0% vs 40.8%, p<0.001; Table 1). In the unadjusted analyses, CZP pts demonstrated increased pharmacy usage (68.7 vs 56.1 fills per pt per yr, p<0.001), but reduced physician office visits (19.8 vs 21.9, p<0.001) and OP hospital-based services (4.4 vs 4.9, p=0.221) compared to IFX pts, resulting in greater overall pharmacy costs but lower medical expenditure than IFX patients (p values <0.001; Figure 1A). In adjusted analyses, MV models controlling for patient and treatment characteristics revealed that prior biologic use was associated with more office visits (p<0.001), OP visits (p<0.001), ER utilization (p<0.001), and elevated total medical costs (p<0.001). Despite the CZP cohort having more biologic-experienced pts, CZP treatment was associated with fewer physician office (p<0.001; Table 2) and OP (p<0.001; Table 2) services compared to IFX pts, but a greater pharmacy spend (p<0.001; Figure 1B). However, CZP treatment was associated with reduced total healthcare costs (p<0.001), with IFX pts incurring over $4,000 per pt per yr more than CZP pts ($46,908 vs $42,867, p<0.001; Figure 1B).
Conclusion: Despite the CZP-treated RA population having a higher rate of prior biologic use, which has been correlated with more severe disease,2 annual total healthcare costs were higher for IFX-treated RA pts. MV models controlling for demographics and baseline HRU revealed that treatment with CZP was associated with a $4,000 saving per pt per yr compared to treatment with IFX.
References:
1. Tkacz J. J Manag Care Spec Pharm 2016;22(Suppl10):S106(Abstract M12)
2. Harrold L. Arthritis Rheumatol 2016;68(Suppl10):3489–91
To cite this abstract in AMA style:
Tkacz J, Lee E, Low R, Stark J, Yassine M, Brady B. Healthcare Service Utilization and Costs of Certolizumab Pegol Versus Infliximab Treatment in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/healthcare-service-utilization-and-costs-of-certolizumab-pegol-versus-infliximab-treatment-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/healthcare-service-utilization-and-costs-of-certolizumab-pegol-versus-infliximab-treatment-in-patients-with-rheumatoid-arthritis/