Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: To determine health literacy, medication adherence, and quality of life (QOL) of uveitis patients in order to understand how to deliver better and improved quality of care given uveitis patients’ multidisciplinary needs.
Methods: We performed a cross-sectional quality improvement study of uveitis patients treated at an outpatient ophthalmology clinic at a 953-bed county hospital in Atlanta, Georgia. A prospective assessment of health literacy using the Short Assessment of Health Literacy survey (SAHL), adherence using the Beliefs about Medicine Questionnaire (BMQ), and QOL using the 12-item Short Form Health Survey (SF-12) were obtained from 60 consecutive patients, as well as baseline data on uveitis diagnosis and etiology.
Results: Demographics: 57% of patients were women and 80% identified as Black. 42% of patients had schooling beyond high school. 32% of patients earned < $5,000 in annual household income, and 79% earned < $30,000. 27% of patients were uninsured.
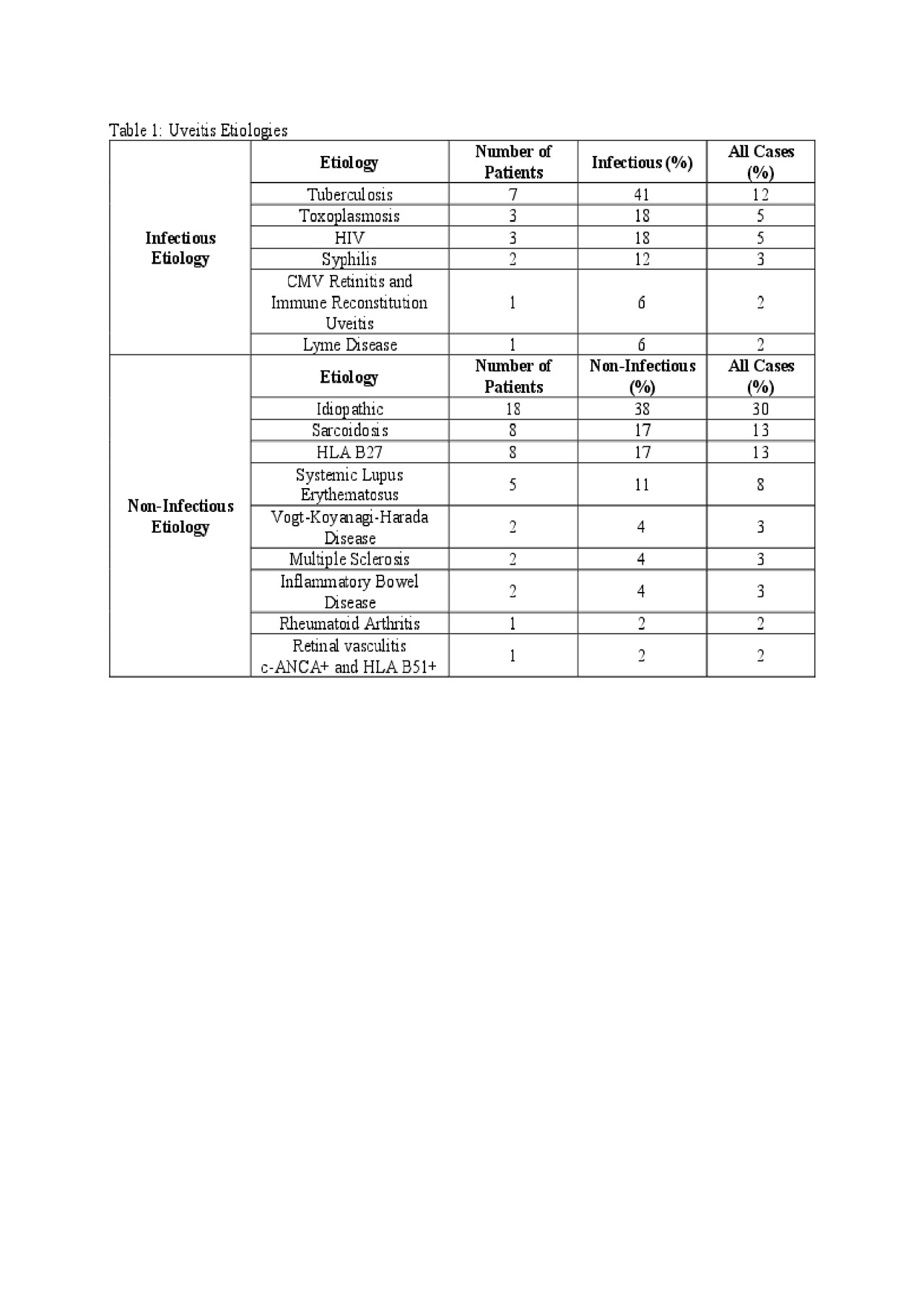
Uveitis description and etiology: 70% of cases were bilateral and 43% were anterior in location. 25% were infectious etiologies and 51% were related to inflammatory disease or markers.
Health Literacy: 43% of patients had poor health literacy. Mean SAHL was significantly lower for those with less schooling (p< 0.0001).
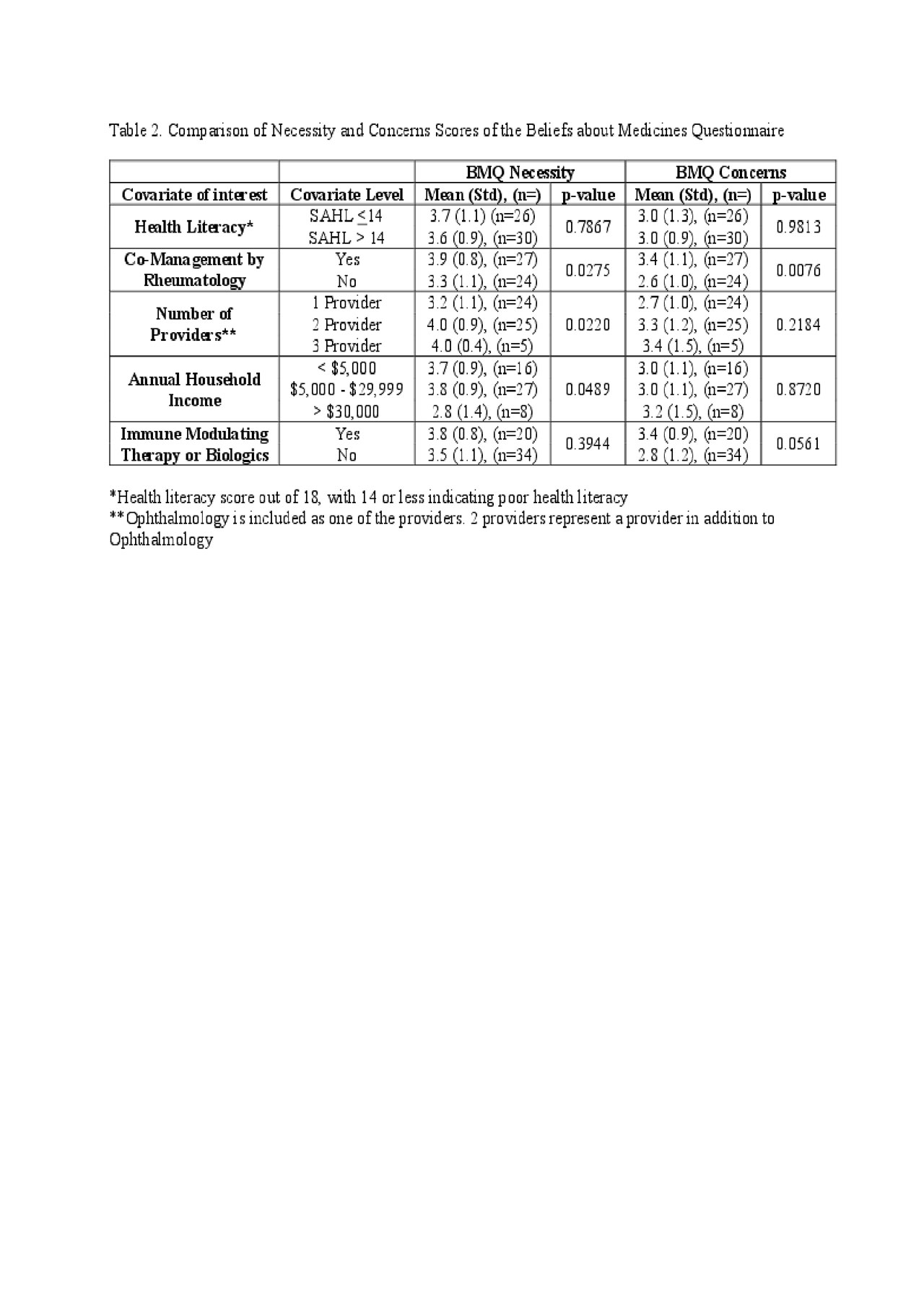
Beliefs about Medicines: Mean necessity scores (3.7/5) were higher than concerns scores (3.2/5). Necessity scores were higher for multiple providers (p=0.0220) as well as those co-managed by rheumatology (p=0.0275). Concerns scores were higher (p=0.0076) for patients co-managed by rheumatology.
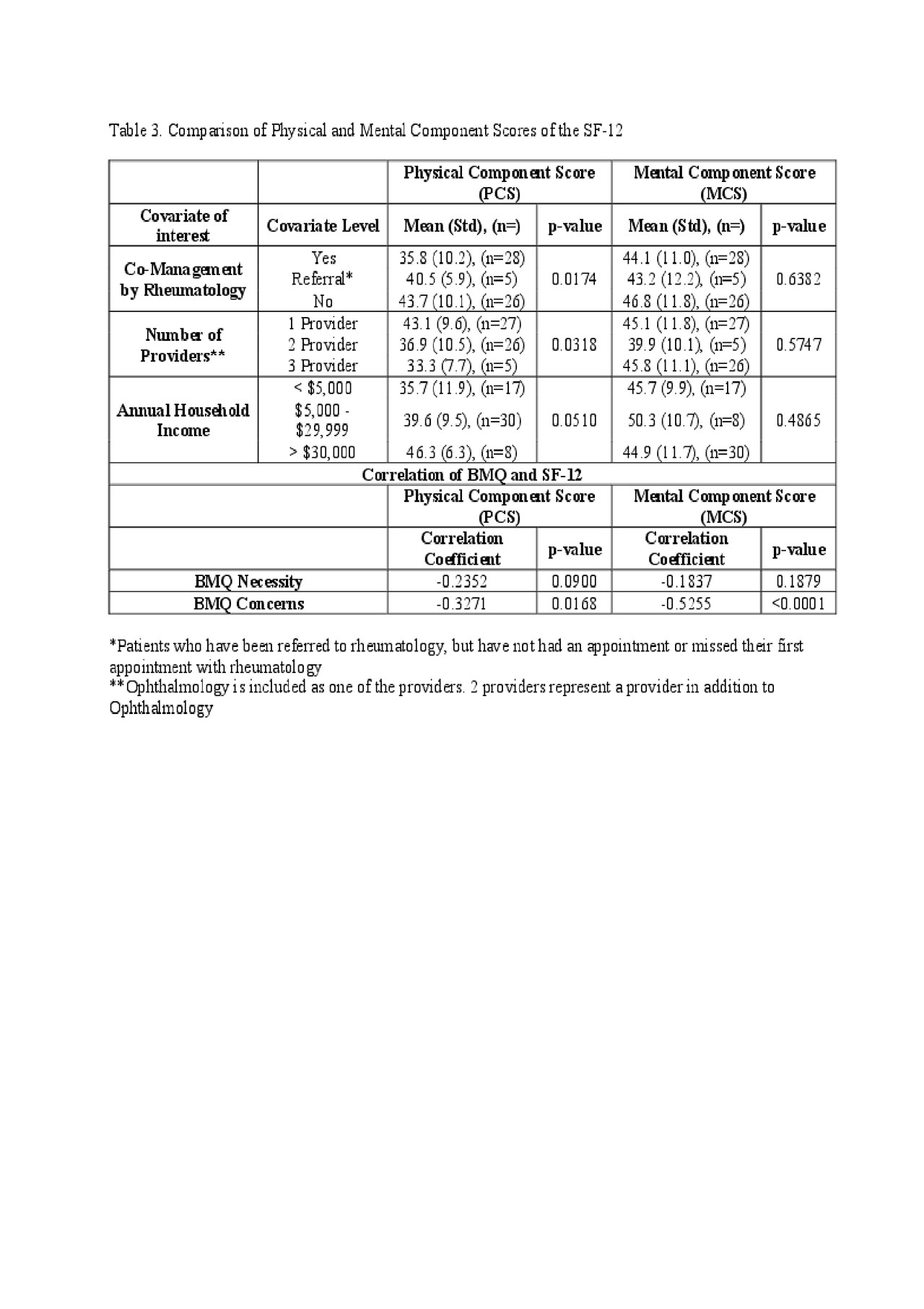
Quality of Life (QOL): Uveitis patients scored lower than the general US population for physical (p< 0.0001) and mental QOL (p=0.002). Physical QOL was lower for patients co-managed by rheumatology (p=0.0174), those managed by multiple providers (p=0.0318), or those on immune modifying therapy (p=0.0345).
Conclusion: Uveitis patients reported many barriers to care, have significantly poorer QOL compared to normal subjects, and have poor health literacy. Despite strong perceptions of treatment necessity there were also treatment concerns. Rheumatology patients have worse physical QOL but indicated increased adherence. Co-management with other specialties and patient education may be beneficial in improving medication adherence and QOL.
To cite this abstract in AMA style:
Mueller C, O'Keefe G. Health Literacy, Adherence, and Quality of Life of Uveitis Patients [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/health-literacy-adherence-and-quality-of-life-of-uveitis-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/health-literacy-adherence-and-quality-of-life-of-uveitis-patients/