Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Approximate 7.2% Chinese were infected with hepatitis B virus (HBV), and the prevalence of concurrent HBV carriers in Chinese rheumatoid arthritis (RA) patients was 9.4% (Lie D, et al. Clin Rheumatol, 2013). Antiviral prophylaxis is recommmended for HBV carriers with RA during DMARDs treatment except hydroxychloroquine by ACR 2008, similar to the professional guideline of Asian Pacific Association for the Study of the Liver. However, antiviral prophylaxis is not commonly used in China due to high economic burden, poor patient compliance and the efficacy/safety of antiviral drugs. This study was to explore the risk of DMARDs associated HBV reactivation and consequent hepatitis in different HBV carriers with RA and the efficacy of antiviral prophylaxis.
Methods: HBV carriers with RA (HBsAg+ and normal transaminases) were enrolled from July 2007 to December 2012 and patients with ≥6-month’s follow-up were qualified for analysis. HBV carriers were divided into inactive group (either HBeAg or HBV-DNA negative) and chronic group (HBeAg and/or HBV-DNA positive). HBV reactivation was defined as a 10-fold rise in HBV-DNA compared to baseline or switch from undetectable to detectable.
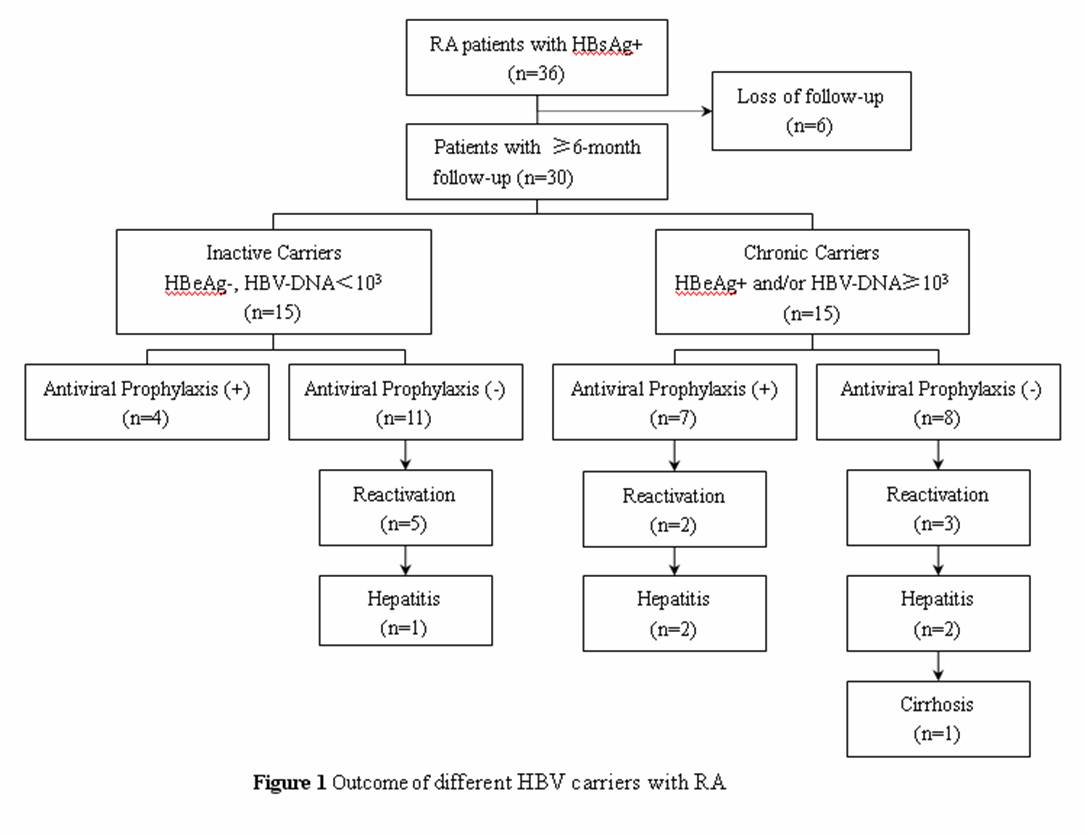
Results: (1) 36 HBV carriers with RA were enrolled and 6 of them failed to complete the ≥6-month’s follow-up due to home migration or conversion to Chinese herbal therapy. Among the qualified 30 patients, 77% were female, mean age was 48 years (range, 17~80), median disease duration was 19 months (range, 1~360) and mean DAS28 was 4.6 (range, 1.7~7.6). There were no significant differences between inactive group (n=15) and chronic group (n=15) in age, gender, disease duration, disease activity (all P>0.05). (2) During a median follow-up period of 12 months (range, 6-69months), 87% patients received low-dose corticosteriods, 100% received MTX, 17% received leflunomide, 50% received sulfasalazine and 67% received hydroxychloroquine. All patients were treated with combination DMARDs therapy with or without low-dose corticosteriods. (3) The outcome of different HBV carriers with RA was shown in figure 1. 33% developed HBV reactivation and 17% developed the consequent hepatitis. Survival curves showed patients in chronic group tend to develop HBV reactivation and consequent hepatitis earlier than in inactive group (figure not shown). (4) Multivariate logistic regression analyses showed the risk factors of HBV reactivation were leflunomide (OR: 6.376, 95% CI: 1.063-38.227) and poor patient compliance of antiviral drugs (OR: 21.140, 95% CI: 1.309-341.467), the risk factor of the consequent hepatitis was past history of acute hepatitis (OR: 17.334; 95% CI: 1.225-245.267).
Conclusion: Our preliminary results suggest that HBV carriers with RA should avoid leflunomide and antiviral prophylaxis should be prescribed for either chronic or inactive HBV carriers during DMARDs treatment, especially for patients with past history of acute hepatitis.
Disclosure:
L. Dai,
None;
A. Q. Liang,
None;
Y. Q. Mo,
None;
J. D. Ma,
None;
L. F. Chen,
None;
D. H. Zheng,
None;
L. J. Zhu,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hbv-reactivation-and-consequent-hepatitis-in-rheumatoid-arthritis-patients-with-different-hbv-carring-state-a-clinical-observation-follow-up/