Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with skin psoriasis (Pso) have an increased risk of developing psoriatic arthritis (PsA) (6-42%) compared to the general population (0.02-0.42%) [1]. Early diagnosis is crucial to initiate treatment, prevent structural damage, and preserve physical function. However, diagnosing PsA is challenging in the absence of arthritis during clinical visits [2]. Previous studies have shown similarly impaired hand function in Pso patients compared to those with PsA [3]. This study aims to evaluate the risk of PsA development based on clinical scores, quality of life measures and disability indices and hand function.
Methods: Data from two study cohorts were pooled for this analysis: adults with dermatologist-diagnosed skin Pso were recruited in the outpatient clinics of the Departments of Internal Medicine 3 – Rheumatology and Immunology and Dermatology, Universitätsklinikum Erlangen, Germany after giving written informed consent (FAU ethics approvals #125_16B). Hand function at baseline was evaluated using isometric grip strength test (dynamometer) and the fine-motor skill Moberg Picking-Up Test. Subjective hand function was assessed via the Michigan Hand Questionnaire (MHQ), overall disability using the Health Assessment Questionnaire (HAQ), quality-of-life by Short Form-36 (SF-36) questionnaire, and physical activity levels with the International Physical Activity Questionnaire (IPAQ). Clinical disease activity scores were retrospectively retrieved from patients records. The cohorts were followed prospectively for PsA onset or the latest available observation. For statistical analysis overall PsA-free survival and covariates were assessed, by comparing baseline characteristics of those who developed PsA and those who did not. In addition, hazard ratios (HR) of hand function measures on the risk of PsA development were assessed.
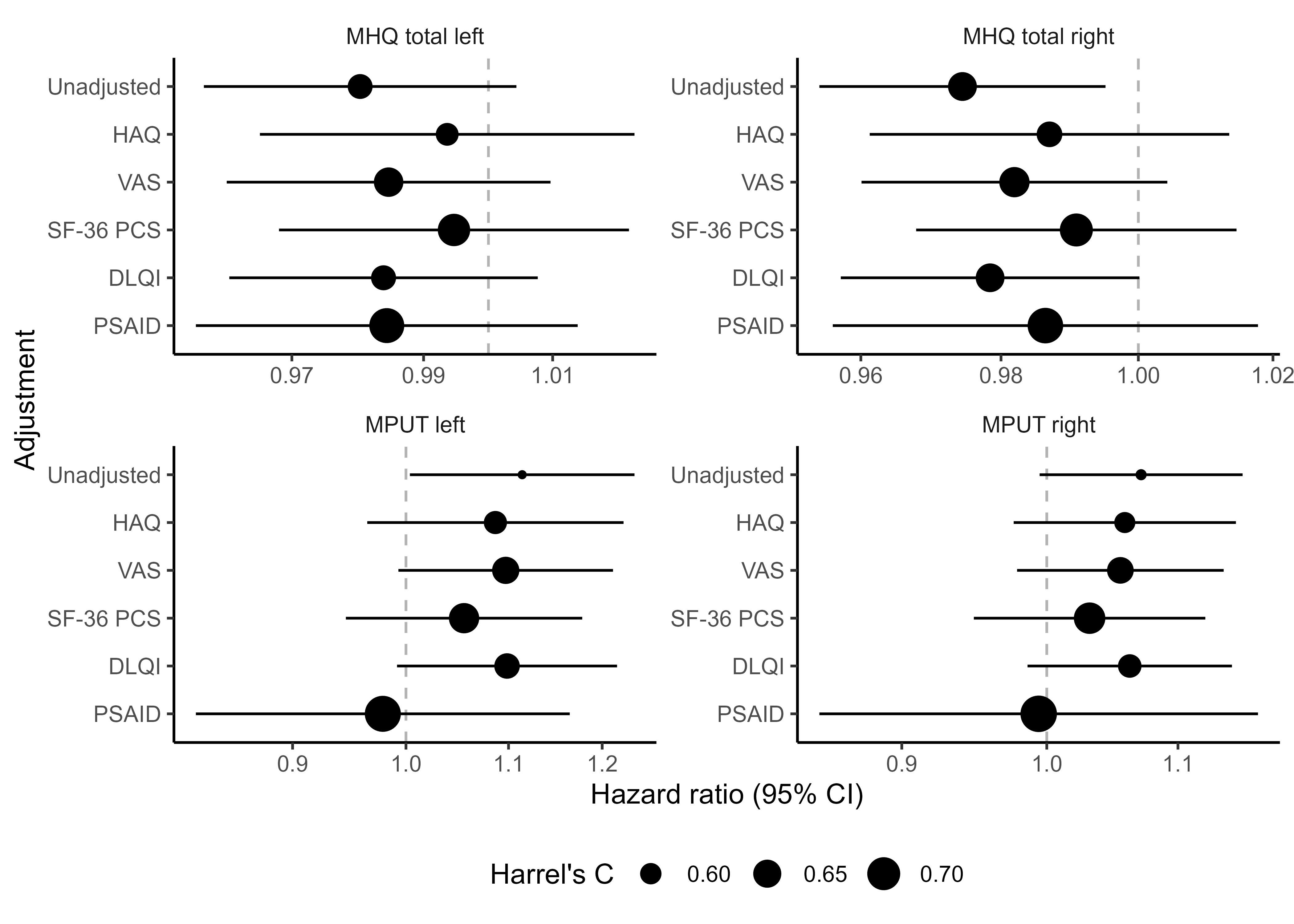
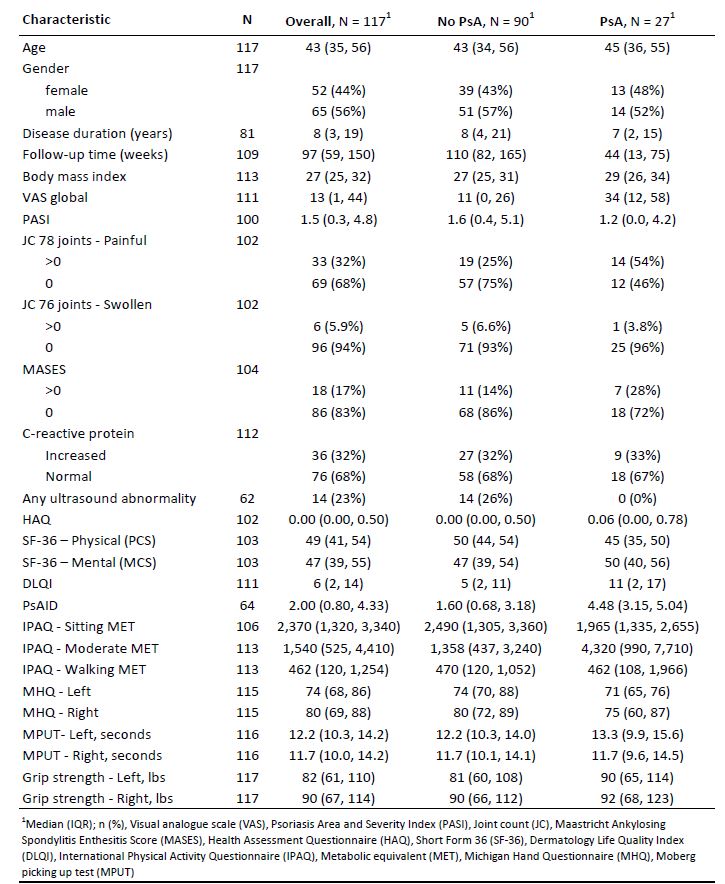
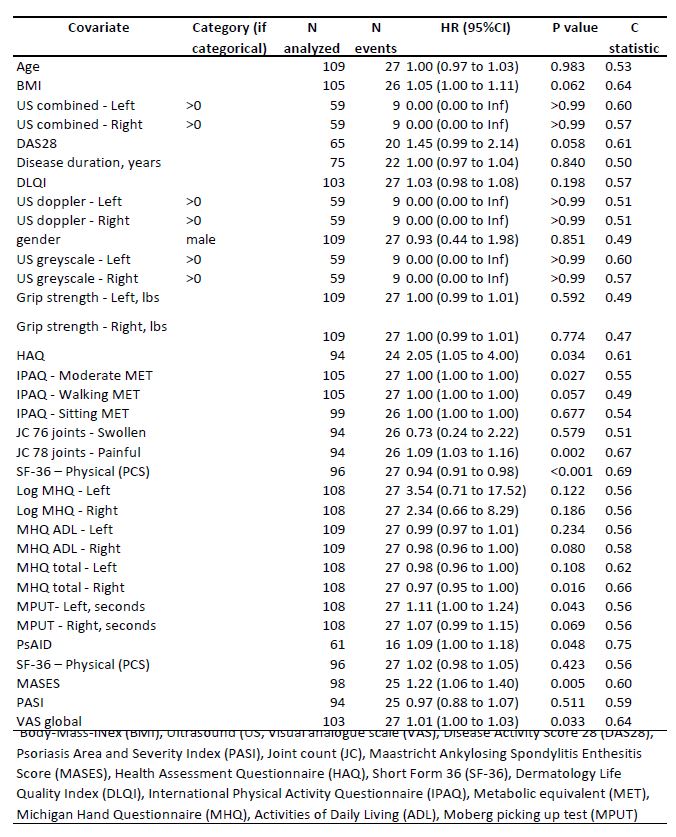
Results: We included 117 patients with Pso at baseline in the analysis, of whom 27 developed PsA within 1-312 weeks of follow-up (Tab. 1). Unadjusted hazard ratios indicated significant associations for PsA development for the following scores (HR, 95%CI): higher HAQ (2.05, 1.05 to 4.00), Psoriatic Arthritis Impact of Disease (PSAID) (1.09, 1.00 to 1.18), Maastrich Ankylosing Spondylitis Enthesitis (1.22, 1.06 to 1.40), Visual Analogue Scale global (1.01, 1.00 to 1.03), number of tender joints (0.73, 0.24 to 2.22), lowerSF-36 physical component scale (0.94, 0.91 to 0.98) and MHQ total right-hand (0.97, 0.95 to 1.00) (Tab. 2). HR for hand function measures adjusted by disability/quality of life indices showed highest influence by PSAID and SF-36 PCS (Fig. 1).
Conclusion: General well-being and musculoskeletal status scored via HAQ, PSAID Score, the SF-36 physical component scale, painful joint/entheseal counts and global disease activity ratings are associated with PsA development. Hand function also showed an association with the risk of developing PsA that was offset after adjustment for overall function and quality of life, indicating a capability to reflect overall function as a candidate predictor for the risk of arthritis development in Pso patients.
To cite this abstract in AMA style:
Coppers B, Bayat S, Tascilar K, Bohr D, Valor L, Simon D, Fagni F, Corte G, Hueber A, Morf H, schönau v, Sticherling M, manger e, liehr s, Rech J, Schett G, Kleyer A, Liphardt A. Hand Function and Development of Psoriatic Arthritis in Skin Psoriasis Patients, a Prospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/hand-function-and-development-of-psoriatic-arthritis-in-skin-psoriasis-patients-a-prospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hand-function-and-development-of-psoriatic-arthritis-in-skin-psoriasis-patients-a-prospective-cohort-study/