Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with SLE experience substantial health disparities. Studying the effect of spatial context on health outcomes has become a focus in health disparities research. The CDC Social Vulnerability Index (SVI) characterizes census tracts by individual dimensions of social vulnerability, which create a cumulative SVI capable of identifying communities where social determinants lead to higher levels of morbidity and mortality. We sought to understand the level of social vulnerability where patients with SLE reside and determine if specific dimensions of social vulnerability were associated with disease activity and prednisone utilization.
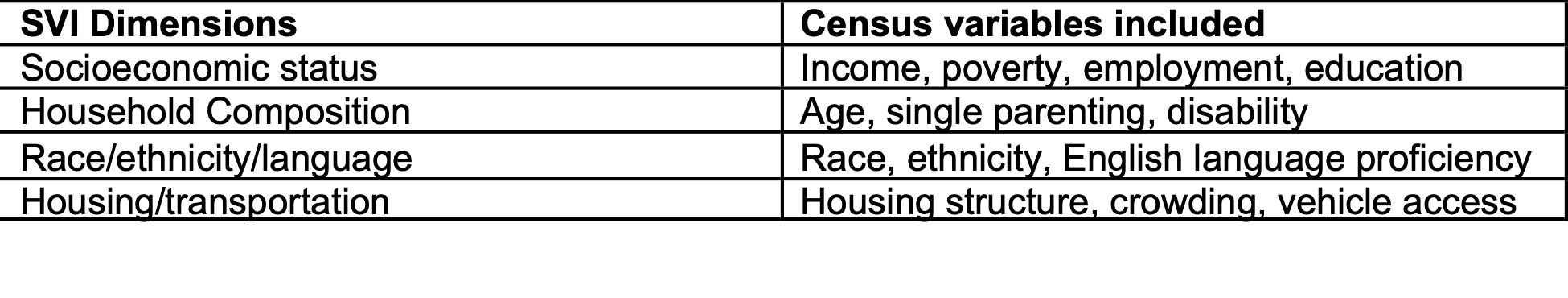
Methods: At the Washington University Lupus Clinic, 324 consented subjects who met either ACR or SLICC classification criteria for SLE were enrolled and longitudinally assessed from April 2014 to August 2020. Participant addresses were recorded for each clinic visit. The census tract code was determined for the address listed for each patient’s index visit which corresponds to a SVI available in the CDC database. Participants with addresses which did not correspond to a census tract code were excluded. SVI ranges from 0 to 1 with 1 being the most vulnerable; any tract with a SVI greater than the mean of 0.5 can be seen as a socially vulnerable area. Specific dimensions of SVI (socioeconomic status, household composition, race/ethnicity/language, and housing/transportation) are further elaborated in Table 1.Prednisone dosing was organized into four categories (none, >0-7.5 mg, 8-20 mg, >20 mg). SLEDAI-2000 Responder Index-50 (S2K RI-50) assessed SLE disease activity ( >4 indicated active SLE). A multinomial logistic regression model analysis was used to determine association.
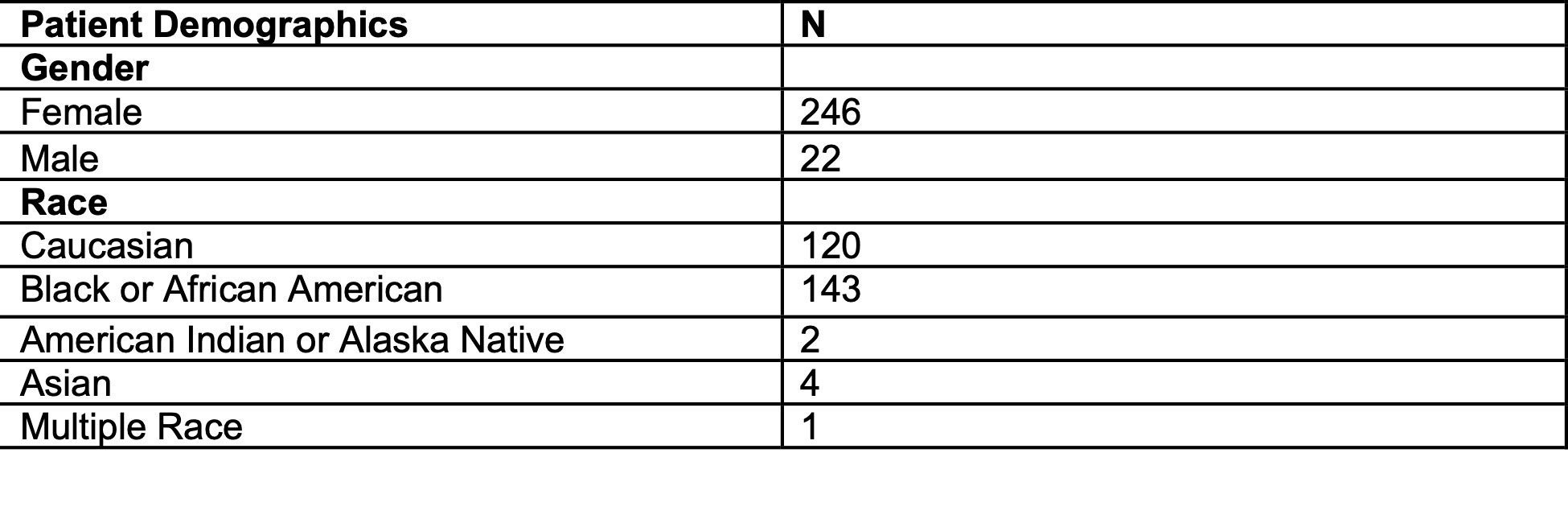
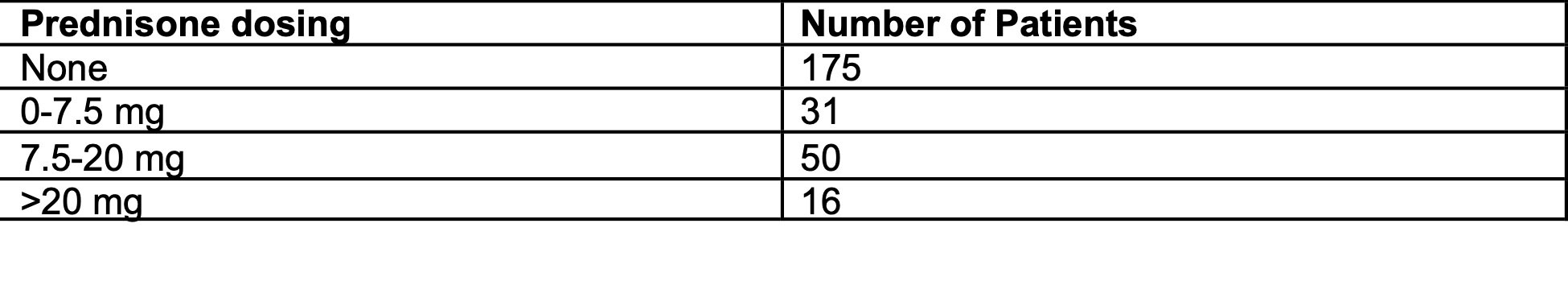
Results: The number of patients with SVI and prednisone data available was 272 patients (Table 2). There was no significant correlation between cumulative SVI and disease activity (OR 1.15, 95% CI=0.67-1.99, p=0.6128). When examining prednisone utilization, 175 patients were not prescribed any prednisone at their index visit while 66 were on supraphysiologic doses (Table 3). Average cumulative SVI was 0.508. Compared to patients with invulnerable cumulative SVI, vulnerable patients were 2.31 times as likely to have higher dose of prednisone (95% CI 1.36-3.92; p=0.0019). Of the specific dimensions, patients vulnerable in terms of socioeconomic status (OR 2.47, 95% CI 1.43-4.27, p=.0012) and household composition (OR 1.57, 95% CI 1.39-4.05, p=0.0016) were also more likely to have higher doses of prednisone. Patients vulnerable in terms of race/ethnicity/language (OR 1.57, 95% CI 0.92-2.68, p=0.095) and housing/transportation (1.08, 95% CI 0.65-1.80, p=0.7537) were not statistically significantly likely to have higher doses of prednisone.
Conclusion: Patients who live in more socially vulnerable areas are more likely to be prescribed higher doses of prednisone, specifically patients vulnerable in terms of socioeconomic status and household composition. This is worrisome as this likely will contribute to a higher burden of damage. Consistent with other findings, our work highlights that access to social determinants is associated with health inequities.
To cite this abstract in AMA style:
Som A, McMorrow L, Chen L, Sen D, El-Qunni A, Baker E, Kim A. Greater Social Vulnerability Associates with Greater Glucocorticoid Use in Patients with SLE [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/greater-social-vulnerability-associates-with-greater-glucocorticoid-use-in-patients-with-sle/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/greater-social-vulnerability-associates-with-greater-glucocorticoid-use-in-patients-with-sle/