Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: More than 130 cases of gout of the spine have been reported, with presenting symptoms including acute back pain, neuropathy, and spinal compression; diagnosis is usually based on imaging identification of a mass, followed by tissue confirmation of monosodium urate (MSU) deposition.(Toprover et al. Curr Rheum Rep. 2015.) It is likely that many more cases of gout involve the spine in an asymptomatic manner, or with non-specific back symptoms that are never formally diagnosed.
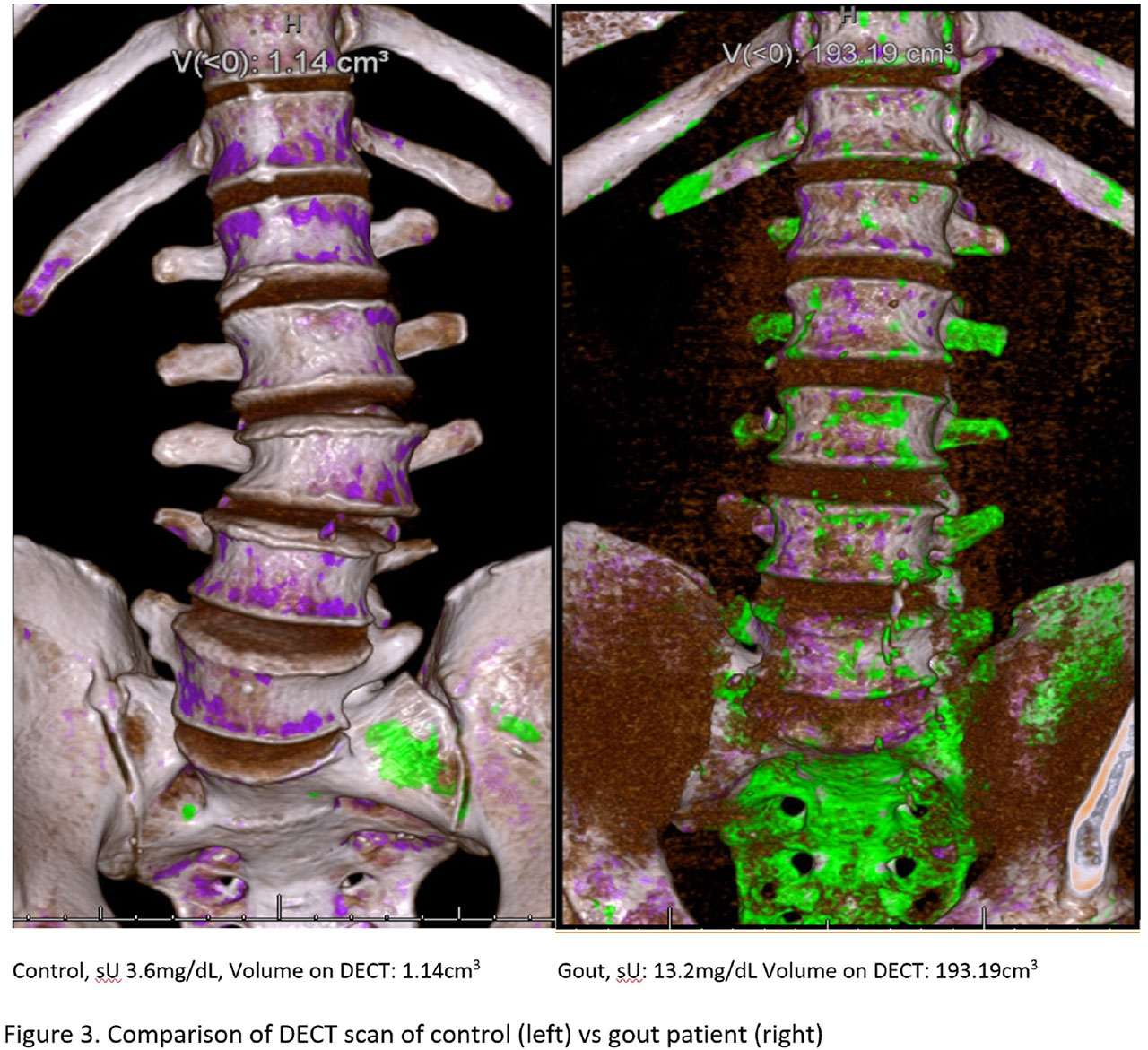
Methods: Using dual-energy CT (DECT), our study aims to determine the prevalence and extent of urate deposition in the lumbosacral spines of patients with clinical tophaceous gout, vs non-tophaceous gout vs control subjects without gout. We are recruiting 25 controls, 25 non-tophaceous and 25 tophaceous gout patients, 50-80 years old. Exclusion criteria include known pseudogout, RA, spondyloarthropathy or active spinal malignancy. All gout subjects meet current ACR/EULAR classification criteria, and have an entry serum urate (sU) of >6.8 mg/dL, or sU >6.0 mg/dL on ULT for < 6 months. Demographics, gout history, back pain data (including Aberdeen back pain scale), sU, ESR, and CRP are collected. Subjects undergo DECT of the lumbosacral spine to assess for MSU deposition.
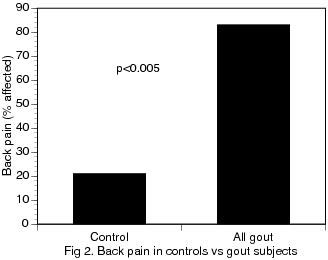
Results: To date, 32 subjects have completed the study: 14 controls, 14 non-tophaceous and 4 tophaceous gout subjects. For these preliminary evaluations, all gout subjects (n=18) are pooled together. To date, all recruited subjects are male. All control subjects identify as white; gout subjects identify as white (61.1%), Black (33.3%) or Hispanic (5.5%). Control and gout subjects have similar mean age in years (controls, 61±1.0 vs gout, 63.3±1.5), but differ in serum creatinine (controls, 1.0±0.1 mg/dL vs gout, 1.5±-0.2 mg/dL, p=0.02). Mean sU is higher in the gout group (controls, 5.3±0.2 mg/dL vs gout, 8.4±0.4 mg/dL, p< 0.05). Gout patients have higher CRP (controls, 1.8±0.5 mg/L vs gout, 9.6±3.3 mg/L, p=0.05), ESR (controls, 11.5± 2.6 mm/h, vs gout, 22.3±4.3mm/h, p=0.06), and MSU deposition in the spine (controls, 2.3 ± 0.2 cm3 vs gout, 15.5±10.5 cm3, p=0.28). When a single outlier gout subject with very high sU and extensive spinal MSU was excluded, spinal MSU deposition between controls and gout patients became significant (controls, 2.3±0.8 cm3 vs gout, 5.0±1.0 cm3, p=0.02). Gout patients reported more back pain (controls, 21% vs gout, 83%, p< 0.005) and greater back pain scores (controls, 4.1±1.6, vs. gout, 10.5±3.4, p=0.12). When plotted against sU, spinal MSU volumes were proportional to sU for controls (R=0.32) and more strongly for gout subjects (R=0.68), suggesting the possibility of spinal MSU deposition even in non-gout individuals.
Conclusion: In these preliminary analyses, gout patients had higher inflammatory markers, greater spinal MSU deposition, and increased rates and severity of back pain compared with non-gout controls. In all patients, spinal MSU deposition was proportional to sU. These data suggest that MSU deposition in the spine is common among gout patients, is associated with sU level, and may be associated with low back pain.
To cite this abstract in AMA style:
Toprover M, Slobodnick A, Pike C, Oh C, Davis C, Mechlin M, Pillinger M. Gout and Serum Urate Levels Are Associated with Lumbar Spine Monosodium Urate Deposition and Chronic Low Back Pain: A Dual-Energy CT Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/gout-and-serum-urate-levels-are-associated-with-lumbar-spine-monosodium-urate-deposition-and-chronic-low-back-pain-a-dual-energy-ct-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gout-and-serum-urate-levels-are-associated-with-lumbar-spine-monosodium-urate-deposition-and-chronic-low-back-pain-a-dual-energy-ct-study/