Session Information
Date: Sunday, November 7, 2021
Title: Pediatric Rheumatology – Clinical Poster II: SLE, JDM, & Juvenile Scleroderma (0764–0785)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Neonatal lupus erythematosus (NLE) is a passively acquired autoimmune disease in infants, secondary to the transplacental passage of maternal autoantibodies against Ro and/or La. The presence of anti-Ro and/or La antibodies are necessary for NLE, but insufficient for disease suggesting additional risk factors. Genetics may impact NLE risk. We analyzed systemic lupus erythematosus (SLE) susceptibility loci in infants and their anti-Ro antibody positive mothers, with NLE risk and NLE specific manifestations.
Methods: We recruited infants born to anti-Ro positive mothers from the NLE clinic at The Hospital for Sick Children. Infants and mothers underwent genotyping on the Illumina Global Screening Array. Ancestry was genetically inferred from principal components (PCs) and Admixture, or self-reported based on Canada census categories. We created additive non-HLA SLE polygenic risk scores (PRSs) using 70 common SLE-risk SNPs from the largest SLE genome wide association study to date. Outcomes were defined as (1) any NLE, (2) cardiac NLE and (3) cutaneous NLE. We tested the association between SLE PRSs in the infant and in the mother with NLE outcomes, in logistic regression models using Generalized linear Mixed Model Association Tests (GMMAT). GMMAT enables inclusion of first-degree relatives in analyses by accounting for relatedness. In order to examine the degree of discordance between maternal and infant PRS, we regressed the difference between mother and infant PRS on NLE outcomes. Models were adjusted for PCs, prior NLE affected infants, maternal rheumatic disease status and hydroxychloroquine use during pregnancy.
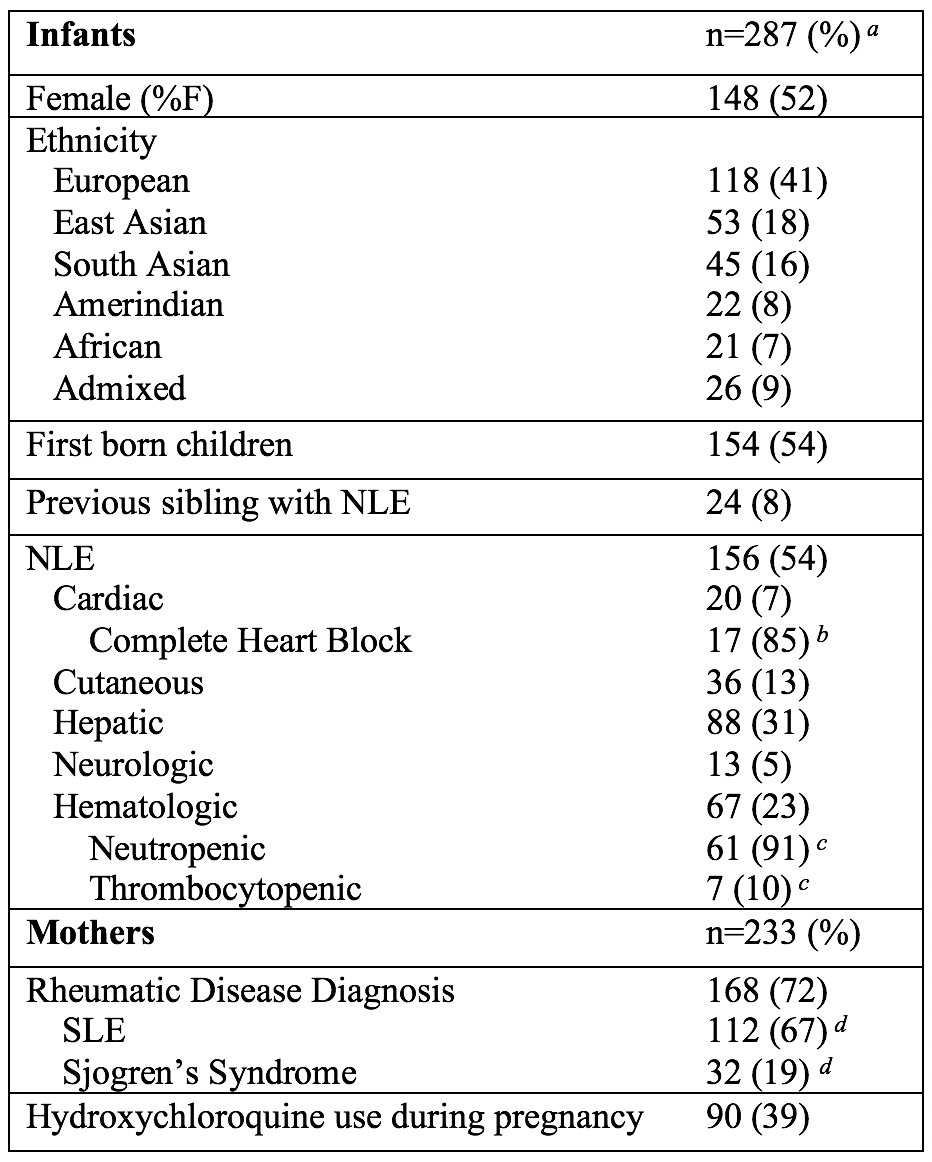
Results: The study included 287 infants born to 233 anti-Ro positive mothers, with 212 genotyped maternal-infant pairs. The majority of infants were European (41%) or East Asian (18%), 52% were female, and 8% had a prior NLE affected sibling. Over half of the infants in the cohort had NLE (54%), including 7% with cardiac NLE and 13% with cutaneous NLE. Of the mothers, 41% were European and 21% were East Asian. A total of 168 mothers (72%) had a rheumatic disease diagnosis and 90 mothers (39%) were on hydroxychloroquine during pregnancy (Table 1).
We did not observe a significant association between infant, maternal or maternal-infant SLE-PRSs and any NLE, cardiac NLE or cutaneous NLE in adjusted GMMAT models (Table 2).
Conclusion: In our multiethnic cohort of infants born to Ro positive mothers, we did not identify a significant association between SLE genetics and risk of NLE or its manifestations. Additional studies are required to replicate our findings.
a Data includes 21 infants with self-reported ethnicity instead of genetically inferred ancestry, and 2 infants without genetically inferred or self-reported ethnicity.
b Percentage of total cardiac NLE cases.
c Percentage of total hematologic NLE cases.
d Percentage of total rheumatic disease diagnoses.
a Models adjusted for PCs, prior NLE affected infants, maternal rheumatic disease and maternal hydroxychloroquine use during pregnancy.
To cite this abstract in AMA style:
Misztal M, Liao F, Diaz T, Baskurt Z, Cao J, Dominguez D, Levy D, Knight A, Hiraki L. Genetics of Neonatal Lupus Erythematosus Risk and Specific Manifestations [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/genetics-of-neonatal-lupus-erythematosus-risk-and-specific-manifestations/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/genetics-of-neonatal-lupus-erythematosus-risk-and-specific-manifestations/