Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriasis and psoriatic arthritis (PsA) are two chronic inflammatory conditions which have similar immunopathological mechanisms which also cause periodontal disease. The association between these conditions is often under-recognized. This study aims to assess the prevalence and severity of periodontitis in psoriasis and psoriatic arthritis, evaluate its correlation with disease activity indices and identify the potential of oral health as a surrogate marker of systemic inflammation.
Methods: In this prospective triple-arm, case-control study, 120 participants were recruited into the study and were equally divided into three groups- healthy subjects as controls, patients with psoriasis and patients with PsA. A detailed periodontal examination was conducted which included measurement of Oral hygiene Index (OHI), gingival bleeding, probing depth (PD), clinical attachment loss (CAL) and missing teeth. Disease activity was measured using Psoriasis Area and Severity Index (PASI) for psoriasis, DAS28 and DAPSA for psoriatic arthritis. Statistical analysis was done using Kruskal Wallis and Spearman’s correlation coefficients and p value < 0.05 was considered as significant.
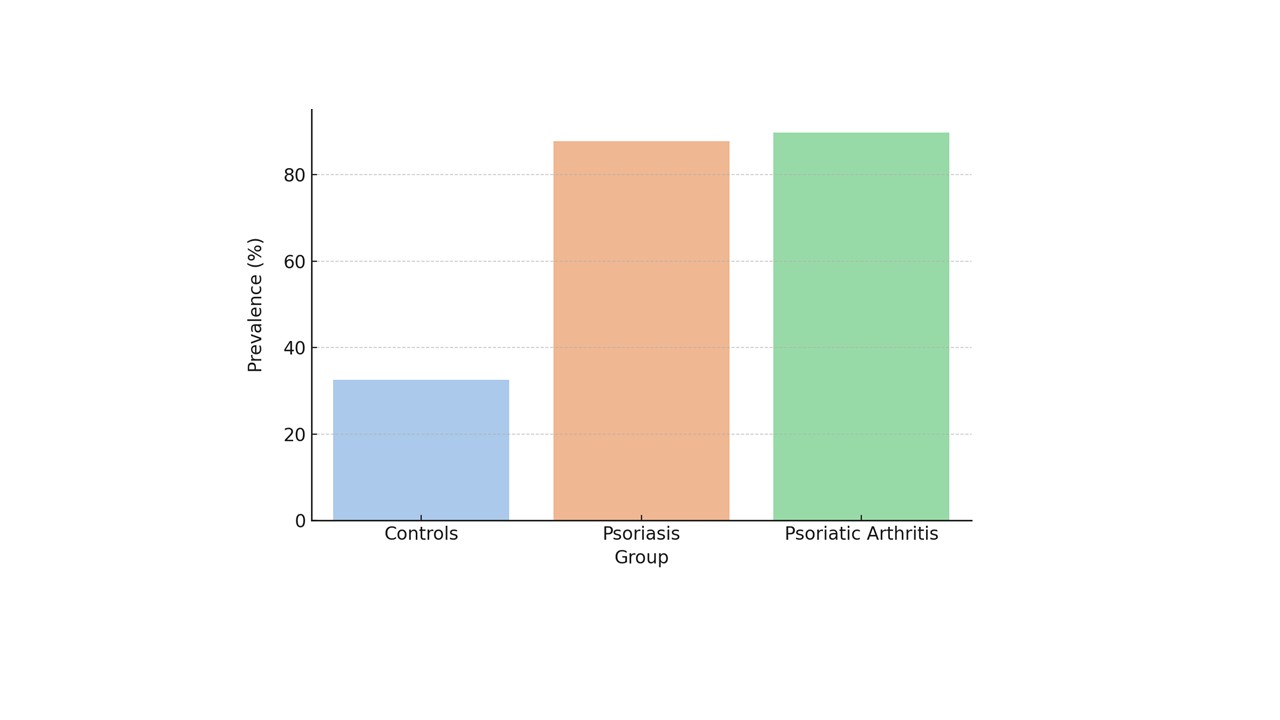
Results: Periodontitis was found to be more prevalent in PsA (89.7%) and psoriasis (87.8%) groups compared to healthy controls (32.5%) (p< 0.001). PsA group demonstrated severe periodontal disease activity with higher OHI, bleeding scores, PD and CAL (p < 0.05 for all). The correlation between indices of psoriasis and PsA with periodontal disease was positive. PASI correlated with bleeding (r=0.460), PD (r=0.338), and CAL (r=0.429), all p< 0.001.DAPSA correlated with bleeding (r=0.439, p< 0.001), PD (r=0.396, p=0.013), and CAL (r=0.358, p=0.025).DAS28 correlated with bleeding (r=0.438, p< 0.001), PD (r=0.325, p=0.043), and CRP (r=0.328, p=0.041) (Figure 2).
Conclusion: This study highlights the striking significant association between periodontal disease and disease activity of psoriasis. The study also highlights the fact that higher disease activity of periodontitis was observed in PsA group. Given the ease of periodontal assessment, it may serve as a non-invasive reflective biomarker of systemic inflammation in patients with PsA and psoriasis. The study also emphasizes the need for early periodontal screening in patients with psoriasis for timely identification and integrated approach of disease management (oral-systemic axis).
To cite this abstract in AMA style:
Chagalakondu g, Parimi V, Anand P. From Plaque to Plaque: Bridging Oral and Systemic Inflammation in Psoriasis and PsA [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/from-plaque-to-plaque-bridging-oral-and-systemic-inflammation-in-psoriasis-and-psa/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/from-plaque-to-plaque-bridging-oral-and-systemic-inflammation-in-psoriasis-and-psa/

.jpg)