Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: We evaluated the real-world frequency and severity of flares and associated costs 1 year post diagnosis in a US cohort with newly diagnosed SLE.
Methods: Adult patients with newly diagnosed SLE were identified using linked Truven Health MarketScan® commercial claims data and IQVIA’s GE Centricity electronic medical record (EMR) database between January 1, 2005 and December 31, 2014. Patients were required to have no prior SLE or lupus nephritis diagnosis during 1 year prior to index date (diagnosis) and ≥1 year of continuous enrollment pre- and post-index date.
Disease severity and flare severity were classified as mild, moderate, or severe during 1 year post diagnosis using a claims-based algorithm, which combined SLE diagnosis, disease activity/SLE-related conditions (eg, end-stage renal disease as severe), medications (eg, oral corticosteroids [CS] ≥60 mg/day as severe), and health service use (eg, hospitalizations, emergency department visits), supplemented with EMRs (1). We evaluated the frequency and severity of flares by SLE severity during the first year post diagnosis. Annualized flare rates and all-cause costs 30, 60, and 90 days after a SLE flare were calculated using 2017 US dollars.
Results: Of 2,227 patients included in this analysis, the average age was 50.2 years; 90.6% were female and 54.4% white. In total, 26.3% (586) of patients were categorized as having mild, 51.0% (1,135) moderate, and 22.7% (506) severe SLE. Prescribed treatments included CS (76.1%), hydroxychloroquine (59.7%), methotrexate (14.7%), and biologics (2.7%).
The annualized flare rate among all SLE patients during the year post diagnosis was 3.45 (SD 1.90) flares. Annualized flare rates increased with disease severity: mild SLE, 2.23 (1.63); moderate SLE, 3.74 (1.73); severe SLE, 4.19 (1.89); P< 0.0001 (Figure 1). Patients with mild SLE did not experience severe flares. A total of 95.1% of all patients with SLE had ≥1 flare, whereas 67.0% experienced 3 or more flares. The proportion of patients who experienced ≥3 flares increased with disease severity (42.0% mild, 74.5% moderate, and 79.6% severe SLE; P< 0.0001).
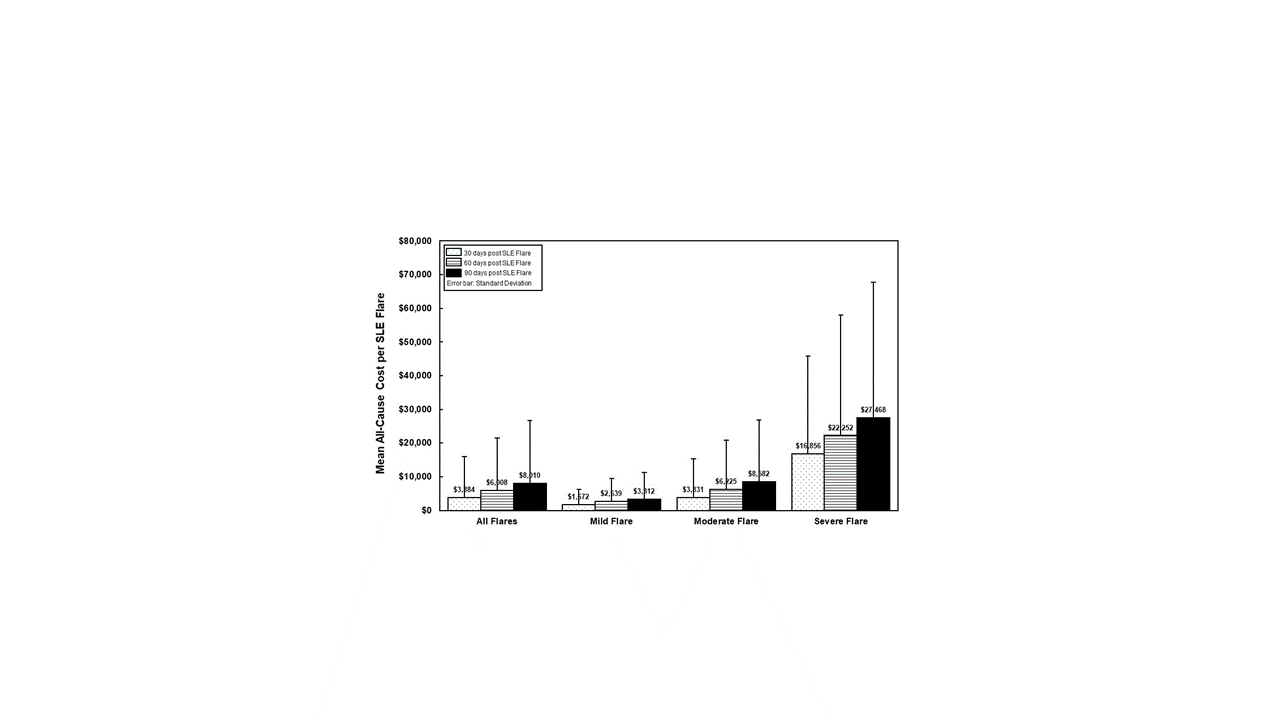
During the initial 30 days after a flare, the total mean all-cause cost of care was $3,884 (SD $12,178), and by flare severity was mild flare $1,672 ($4,566), moderate flare $3,831 ($11,552), and severe flare $16,856 ($29,001); P< 0.0001 (Figure 2). Health care costs following severe flares was 10.1-fold higher compared with mild flares and 4.4-fold higher for moderate flares compared with mild flares. Health care costs continued to increase 60 and 90 days after a flare with increasing flare severity. Inpatient costs were the primary driver of health care cost after a severe flare.
Conclusion: The frequency and severity of flares in patients with SLE increases with disease severity and with an associated significant increase in health care costs. Health care costs continue to increase substantially well into 90 days after a flare. Preventing the occurrence of flares, or reducing the rate and duration of flares, has potential to reduce SLE health care costs and reduce disease progression.
Reference:
- Garris C, et al. J Med Econ. 2013;16:667–677.
To cite this abstract in AMA style:
Jiang M, Desta B, Near A, Wang X, Hammond E. Frequency, Severity and Costs of Flares Increase with Disease Severity in Newly Diagnosed Systematic Lupus Erythematous: A Real-World Cohort Study, United States, 2004–2015 [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frequency-severity-and-costs-of-flares-increase-with-disease-severity-in-newly-diagnosed-systematic-lupus-erythematous-a-real-world-cohort-study-united-states-2004-2015/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-severity-and-costs-of-flares-increase-with-disease-severity-in-newly-diagnosed-systematic-lupus-erythematous-a-real-world-cohort-study-united-states-2004-2015/