Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Antisynthetase syndrome (ASSD) is an autoimmune disease with features including interstitial lung disease (ILD), myositis, inflammatory arthritis, Raynaud phenomenon, and mechanic’s hands.¹ Eight aminoacyl-transfer-RNA (tRNA) synthetase autoantibodies (Ab) have been described so far: Jo-1, PL-7, PL-12, EJ, OJ, YRS, KS, and Zo.¹ Sometimes, additional autoantibodies associated with other autoimmune rheumatologic disorders can be detected in patients with ASSD including ANA, anti-U1-RNP, anti-Sm, anti-ds-DNA, rheumatoid factor (RF), and anti-CCP.2,3,4 In ASSD, the coexistence of these autoantibodies may increase the prevalence of Raynaud phenomenon, dermatomyositis, and deforming arthropathy.2,3,4 Also, copresence of anti-SSA/Ro antibody in ASSD has been variably correlated with more severe interstitial lung disease.2,4,5 We completed a subset analysis evaluating the presence of other (non-tRNA synthetase) antibodies in patients with ASSD.
Methods: We obtained clinical data by retrospective review of electronic medical records from 2004 – 2017. The diagnosis of ASSD was confirmed by a rheumatologist, based on clinical phenotype and presence of one of the following autoantibodies: Jo-1, PL-7, PL-12, EJ, or OJ. Additional autoantibody positivity was determined by positive or negative values. Categorical variables were summarized using frequencies and percentages, and were compared using Pearson’s chi-square tests or Fisher’s exact tests. For all measures, a p-value of < 0.05 was considered significant.
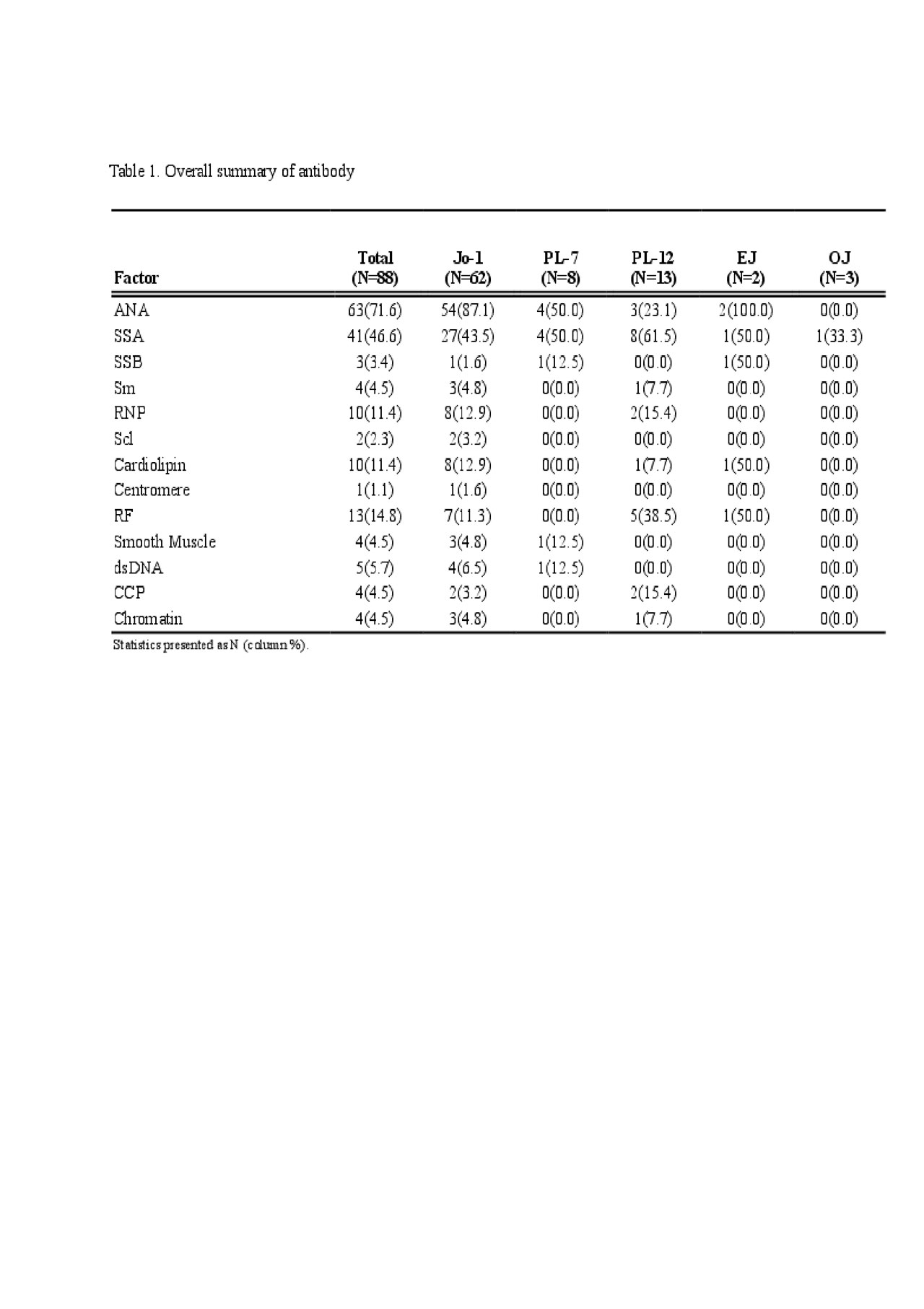
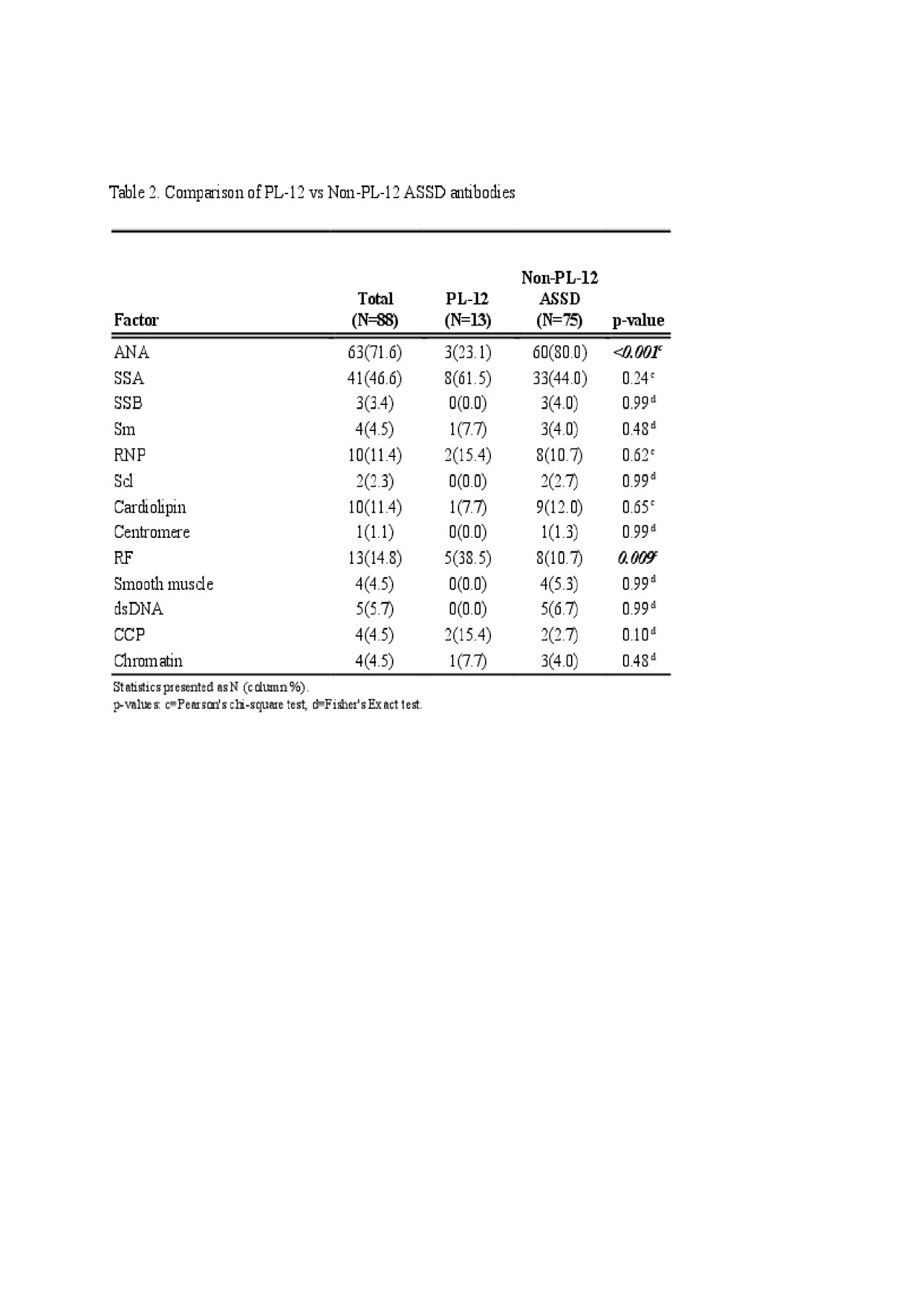
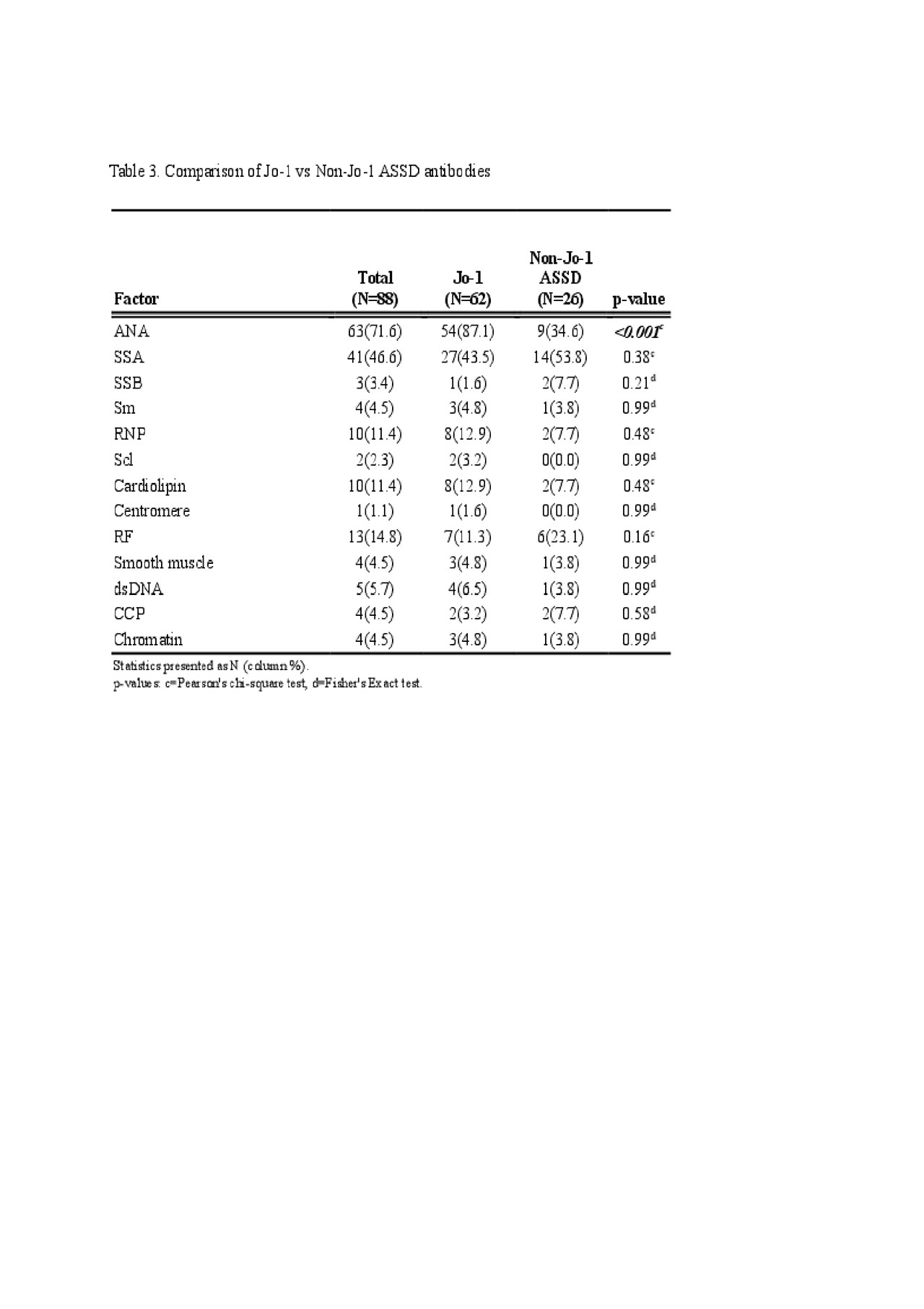
Results: A total of 88 ASSD patients met criteria for inclusion in this study. The mean age was 57 years; 64% were female. The largest subset of patients was positive for Jo-1 Ab (N = 62). A positive ANA was noted in 63/88 patients (71.6%). ANA was more frequently positive in Jo-1 (87.1%) than those with ‘non-Jo-1 ASSD antibody’ (34.6%, p< .001) and PL-12 groups (23.1%, p< 0.001). RF was positive more frequently in PL-12 positive patients 5/13 (38.5%) than both in Jo-1 (11.3%, p=0.015) or ‘Non-PL-12 ASSD antibody’ groups (10.7%, p=0.009). Only 2/15 RF positive patients had radiographic evidence of deforming arthropathy, one of whom was also anti-CCP antibody positive and had erosions. No statistical comparisons were made for PL-7, EJ, and OJ antibodies due to small sample sizes.
Conclusion: Concomitant non-tRNA synthetase antibodies are common in patients with ASSD. Eighty five percent of our ASSD patients had at least one additional non-tRNA synthetase autoantibody, and almost 30% had at least three such additional autoantibodies, the most common ones being ANA, SSA, and RF. The impact of these autoantibodies on the phenotype and prognosis of ASSD patients remains unclear, and additional research is needed in this field.
- Katzap et al. Curr Rheumatol Rep, 13: 175.
- M. Fritzler et al. Journal of Rheumatology, 45 (3) 444-445.
- Cavagna L et al. Medicine (Baltimore); 94(32):e1144.
- Hervier et al. Curr Rheumatol Rep, 15: 349.
- R. La Corte, et al. Autoimmunity, 39:3, 249-253.
To cite this abstract in AMA style:
Katz A, Chatterjee S, Jin Y. Frequency of Concomitant Non-aminoacyl-transfer-RNA Synthetase Autoantibodies in Patients with Antisynthetase Syndrome [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frequency-of-concomitant-non-aminoacyl-transfer-rna-synthetase-autoantibodies-in-patients-with-antisynthetase-syndrome/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-of-concomitant-non-aminoacyl-transfer-rna-synthetase-autoantibodies-in-patients-with-antisynthetase-syndrome/