Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: It is a common misconception that allopurinol should either be held or reduced during gout flares and renal insufficiency. However, current guidelines recommend the continuation of allopurinol during flares as long as an effective anti-inflammatory therapy is in place [Khanna, et al 2012]. Additionally, allopurinol has been shown in recent studies to have no association with worsening renal function or increased risk of allopurinol hypersensitivity syndrome in acute renal insufficiency [Vargas-Santos, et al 2018]. In this retrospective observational study, we assessed the frequency of allopurinol dose reduction or discontinuation in patients with gout who had acute flares during inpatient admissions.
Methods: A clinical database was utilized to query patients with ICD-10 diagnosis of gout with prescriptions for allopurinol, who were admitted to two medical centers from 2014-2019. Patients with acute gout flares during the hospitalization were included in the study. Charts were reviewed for patient demographics, comorbidities, allopurinol dose on admission and discharge, reasons for dose changes, use of flare prophylaxis, rheumatology consultation, and gout flares within three months after discharge. Descriptive statistics were performed for patient baseline characteristics and outcomes. We used Fisher’s exact test to assess for the difference between post-hospitalization gout flares between allopurinol dosage change groups.
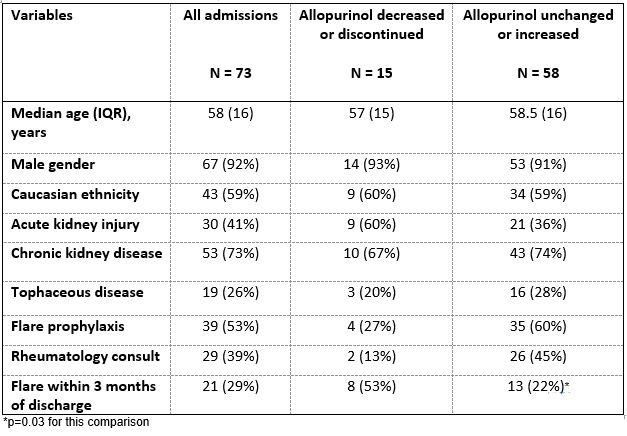
Results: We identified 59 patients with a total of 73 admissions who met inclusion criteria (Table). Of all the admissions, 92% were males with a median age of 58 years. Allopurinol was either reduced or discontinued in 15 admissions (allopurinol reduced group), which comprised 21% of total admissions. Allopurinol was increased or unchanged in the other 58 admissions (comparator group). The proportion of chronic kidney disease was similar between the groups, while there was a greater proportion of admissions with acute kidney injury in the allopurinol reduced versus the comparator group (60% vs. 36%, respectively). The allopurinol reduced group also had a significantly higher rate of gout flares within three months of discharge at 53% compared to the comparator at 22% (P =0.03).
Conclusion: In hospitalized patients with gout who experienced acute flares, allopurinol was decreased or discontinued in nearly a quarter of admissions despite current recommendations. There were significantly more gout flares following these admissions, compared to those in which allopurinol dose was unchanged or increased. Improved clinician awareness of the current gout recommendations, as well as the risks and benefits of allopurinol in the setting of concomitant renal disease, is necessary to improve patient outcomes.
To cite this abstract in AMA style:
Huang I, Bays A, Liew J. Frequency of Allopurinol Dose Reduction in Hospitalized Patients with Gout Flares [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frequency-of-allopurinol-dose-reduction-in-hospitalized-patients-with-gout-flares/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-of-allopurinol-dose-reduction-in-hospitalized-patients-with-gout-flares/