Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Patients with rheumatoid arthritis (RA) have a 60% higher cardiovascular disease (CVD) event risk, yet previously we demonstrated they were ~30% less likely to have hypertension diagnosed. We sought to examine the frequency and predictors of documented hypertension/blood pressure (BP) communication during rheumatology visits for RA patients with undiagnosed and/or uncontrolled hypertension.
Methods: Electronic health record searches from 2004-11 identified RA patients (defined by ICD-9 algorithm) who had uncontrolled or undiagnosed hypertension and who had encounters at 1 of 3 rheumatology clinics. Using Joint National Committee-7 criteria, undiagnosed was defined as ≥3 BPs ≥140/90 mmHg or 2 readings ≥160/100 mmHg without prior diagnosis or antihypertensive medication; BP control was ≥3 consecutive BP’s <140/90 mmHg. We abstracted rheumatology clinic notes from first eligible date for hypertension diagnosis/control through date of hypertension control or end of data. We examined the frequency and predictors of any hypertension communication beyond vital sign documentation. We used multivariate logistic regression to examine the impact of systolic BP stage at a rheumatology visit on the predicted probability (PP) of hypertension communication. Covariates included patient sociodemographics, comorbidity, utilization, visit date, and rheumatologist.
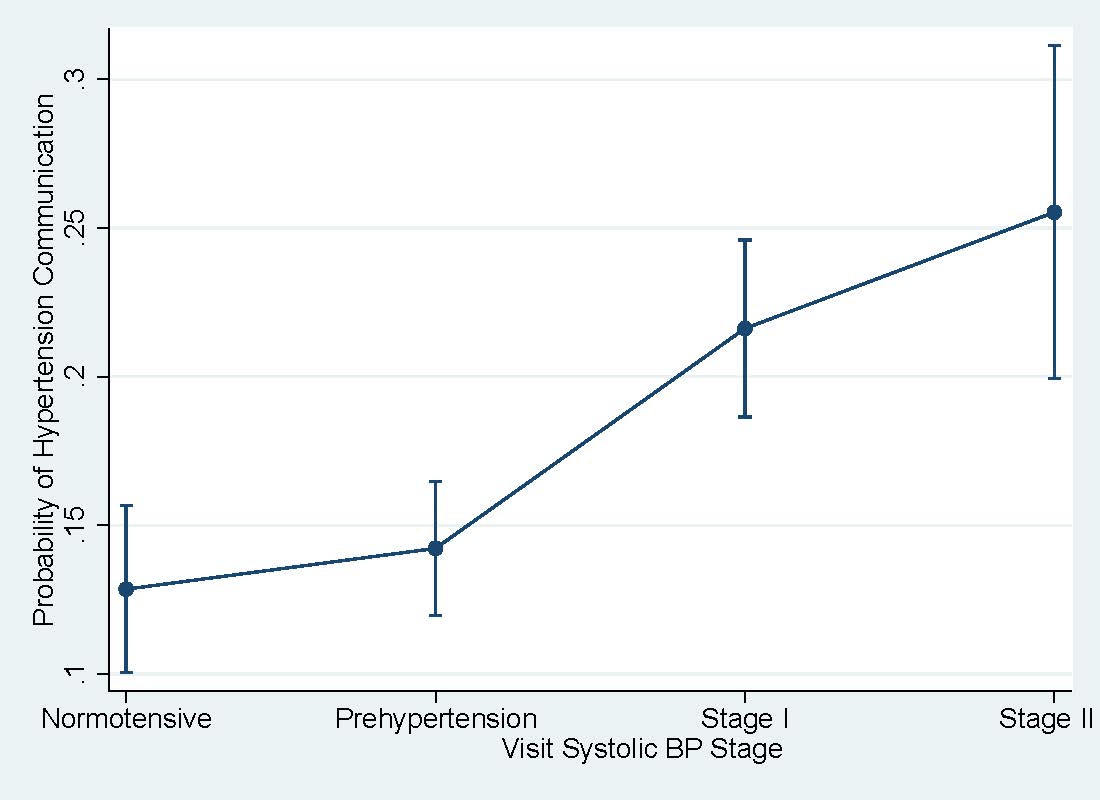
Results: Among 1267 RA patients, 501 were studied who had uncontrolled hypertension, and 232 of the 501 patients met criteria and lacked a hypertension diagnosis. Mean age was 62 years, 76% were female, 11% were current and 35% former smokers, and prior CVD was noted in >20%. In 2677 abstracted visits, BP’s varied with 20% Normotensive (<120 mmHg) at a given visit, 45% Prehypertensive (≥120 - <140 mmHg), 32% with Stage I (≥140 - <160 mmHg) and 11% with Stage II (≥160 mmHg) elevations. Overall 23% of RA visits contained any hypertension communication. After adjustment, even in visits with systolic BPs ≥160 mmHg, only 25% contained hypertension communication (PP 25%, CI 20,31). Compared to Stage I systolic elevations, Stage II elevations did not significantly increase the probability of communication (Figure 1), although both were higher than normotension and prehypertension. When examining other predictors, active tobacco users were least likely to have hypertension communication (PP 12%, CI 8,16).
Conclusion: Despite higher CVD risk, many RA patients had undiagnosed or uncontrolled hypertension. Even with systolic BPs≥160 mmHg only 1 in 4 rheumatology encounters documented communication about hypertension, demonstrating lost opportunities for identifying and managing modifiable CVD risks. Future research should investigate patient and provider role perceptions and other barriers and facilitators of hypertension management to systematically improve CVD prevention in RA patients.
Disclosure:
C. M. Bartels,
None;
H. Johnson,
None;
E. A. Jacobs,
None;
P. McBride,
None;
M. Smith,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-and-predictors-of-hypertension-communication-in-rheumatoid-arthritis-visits/