Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Uveitis is the most frequent extra-articular manifestation (EAM) of spondyloarthritis (SpA). Its prevalence is approximately 30% and increases with the duration of the SpA. The characteristic pattern is anterior, acute, recurrent and unilateral uveitis. However, the frequency and characteristics of uveitis in SpA treated with biological therapy (BT) are unknown. The main target is to describe the frequency and characteristics of uveitis in SpA with BT in a single center.
Methods: Descriptive and retrospective study (January 2003-December 2017) of SpA that develops uveitis in a reference hospital. The epidemiological variables, type of SpA, presence of uveitis and its characteristics, presence of BT at the time of onset and treatment received are collected. For the analysis, frequencies and percentages were used in qualitative variables, and mean and standard deviation (SD) for quantitative variables. Statistical analysis was performed with IBM SPSS v.23.
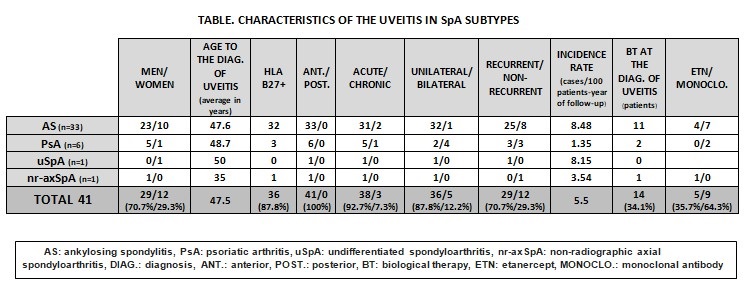
Results: We studied 246 patients with SpA. The subtypes of SpA were: ankylosing spondylitis (AS) (n=125, 50.8%), psoriatic arthritis (PsA) (n=101, 41.1%), undifferentiated SpA (n=13, 5.3%), non-radiographic axial Spa (n=3, 1.2%), enteropathic arthropathy (n=3, 1.2%) and reactive arthritis (n=1, 0.4%). Uveitis was observed in 41 patients (16.7%) after an average time of development of 109.47 (73.9) months of the SpA. The incidence rate was 5.5 cases of uveitis/100 patients-year of follow-up. Men were 70.7% of the patients and the mean age(SD) was 47.4(12.06) years. The HLA B27 was positive in 87.8% of the cases and 41.5% had family history of SpA. Uveitis was observed in 33 patients (80.5%) with AS, in 6 (14.6%) with PsA, in 1 (2.4%) with non-Rx axial SpA and in 1 (2.4%) with undifferentiated SpA. (TABLE) The uveitis pattern was anterior (100%), acute (92.7%), unilateral (87.8%) and in 12.2% bilateral (80% in PsA). At the time of onset of uveitis, the mean ESR was 30.11 mm1ªh, CRP 3.56mg/dL, DAS28 3.66 and BASDAI 3.21. Regarding the diagnosis of SpA, uveitis was after (85.4%), before (12.2%) and simultaneous (2.4%). At the time of the onset of uveitis, 14 patients (34.1%) were with BT (35.7% etanercept, 28.6% infliximab, 21.4% adalimumab, 7.1% golimumab and 7.1% certolizumab). BT was modified in 3 of the cases. The treatment of uveitis was topical (78%), corticoids in oral regimen (57.5%), conventional DMARDs (12.5%), with methotrexate predominating in 60% of cases and BT (15%). The most used biologics were adalimumab (60%) and infliximab (40%).
Conclusion: In our series, uveitis was observed in 16.7% of patients with SpA of which 80.5% were AS and 14.6% PsA. The most frequent uveitis was anterior, unilateral, acute and recurrent. In PsA, the association with HLA B27 was less frequent and was more bilateral. In most cases, the diagnosis was later than the SpA.
To cite this abstract in AMA style:
Calvo Zorrilla I, Guerrero Basterretxea E, Ibarguengoitia O, Montero D, Garcia Vivar ML, Ruíz Lucea E, Torre Salaberri I, Fernandez Berrizbeitia OB, Blanco Madrigal JM, Inchaurbe Pellejero AR, Perez Velasquez CE, Rivera-García N, Allande Lopez Linares MJ, Gorostiza-Hormaetxe I, Galíndez Agirregoikoa E. Frequency and Pattern of the Uveitis in Spondyloarthritis with Biological Therapy [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/frequency-and-pattern-of-the-uveitis-in-spondyloarthritis-with-biological-therapy/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-and-pattern-of-the-uveitis-in-spondyloarthritis-with-biological-therapy/