Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with complex multi-systemic involvement. Herpes zoster (HZ) is caused by the reactivation of latent varicella-zoster virus (VZV) in patients who had been exposed earlier. HZ infection is most commonly seen in elderly and immunocompromised individuals, including those with autoimmune diseases such as rheumatoid arthritis and SLE. In Latin America, information about the estimated frequency and impact of HZ in patients with SLE is scarce. The aim of this study was to assess the epidemiology and clinical characteristics of HZ and to identify factors associated with the first HZ episode in SLE patients.
Methods: GLADEL 2.0 is an observational multi-ethnic Latin-American SLE cohort. Forty-three centers from 10 Latin-American countries enrolled patients ≥18 years of age who fulfilled the 1982/1997 American College of Rheumatology (ACR) and/or the 2012 Systemic Lupus International Collaborating Clinics (SLICC) classification criteria. Baseline demographic, clinical, disease activity (SLEDAI), damage (SLICC/ACR Damage Index), laboratory and treatment data of patients with and without HZ events were examined. Continuous variables are presented as mean (±SD) or median (IQR) and categorical variables as count (percentage). Prevalence was calculated as the proportion of patients with HZ infection out of the SLE patients in the GLADEL 2.0 cohort. Associated factors were identified and logistic regression analysis was performed to examine the adjusted effects of these characteristics on the probability of experiencing at least one episode of HZ infection. The results are presented as ORs and their 95% CIs. P values < 0.05 were considered statistically significant. All analyses were performed with R v4.2.2 (or a later version).
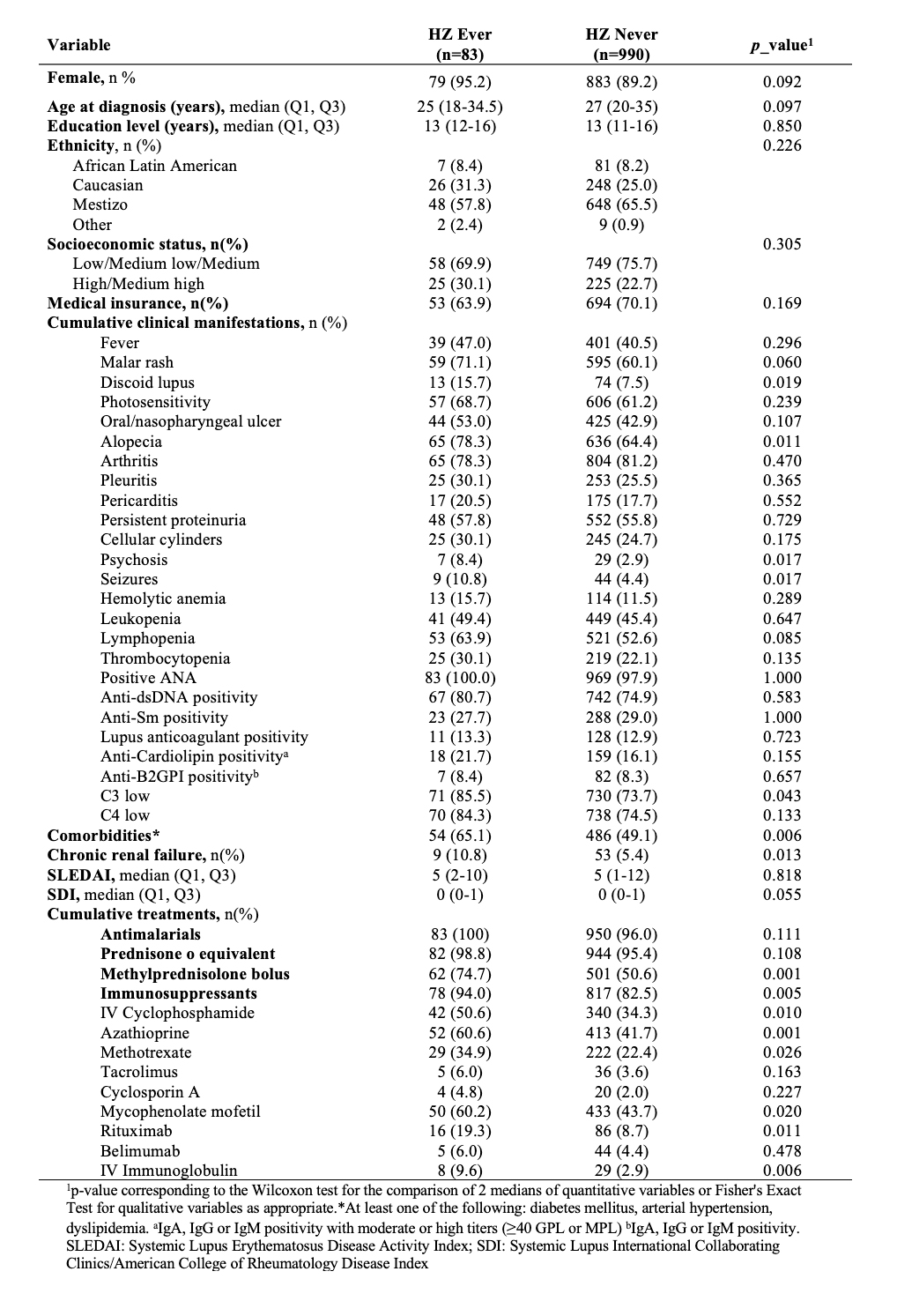
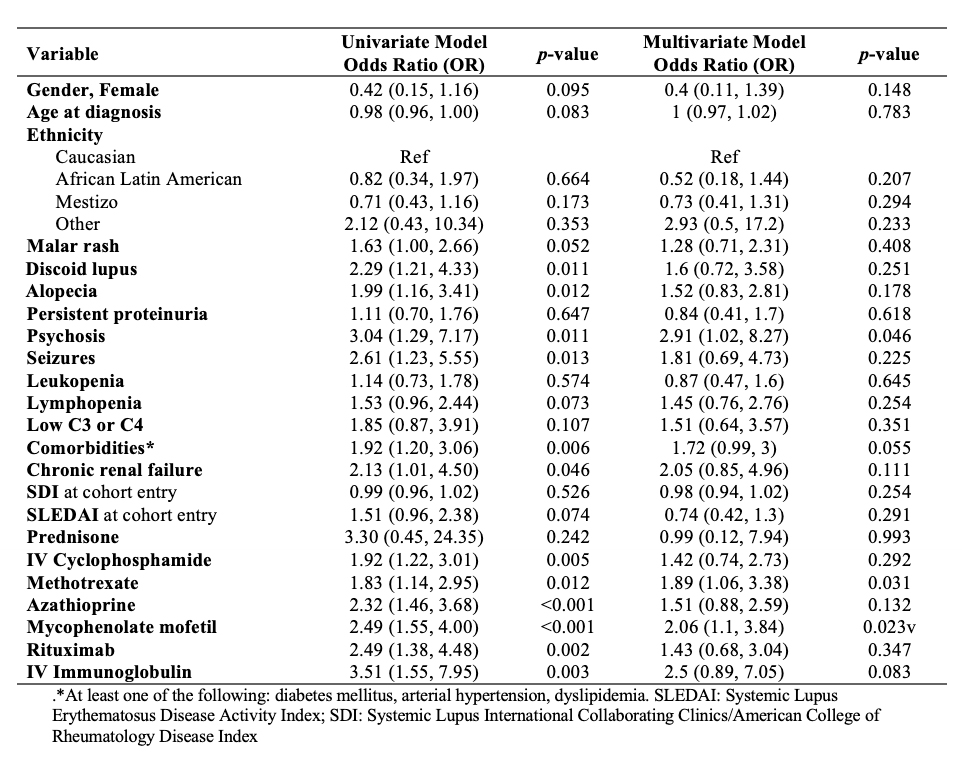
Results: Of the 1083 patients included in the GLADEL 2.0 cohort, 1073 were included in these analyses. A total of 83 HZ events were recorded at the baseline visit. The prevalence of HZ was 8.3% (CI: 6.8%-10.3%). SLE patients with history of HZ infection were more frequently female, with a higher frequency of cutaneous involvement (discoid lupus and alopecia), neurological involvement (psychosis and seizures), low complement, comorbidities and chronic renal failure (table 1). In terms of treatment, they also had a higher frequency of using methylprednisolone boluses, and immunosuppressants (IV cyclophosphamide, azathioprine, methotrexate, mycophenolate, rituximab and IV immunoglobulins). Multivariate analysis found that a history of psychosis and the use of methotrexate and mycophenolate were factors significantly associated with HZ events in these SLE patients (table 2).
Conclusion: In SLE patients from the GLADEL 2.0 cohort, the prevalence of HZ infection was found to be less than 10%. Neurological compromise and the use of immunosuppressants such as methotrexate and mycophenolate were associated with the occurrence of these events. It is important to be aware of the risk of HZ in SLE patients. Future research may be able to establish predictive factors of HZ occurrence in these patients.
To cite this abstract in AMA style:
Nieto R, Hernandez L, Scolnik M, Subils G, Saurit V, Savio V, Arturi V, Kisluk B, González Lucero L, Grageda W, De Los Ángeles Gargiulo M, MONTICIELO O, Duarte A, Borba E, Parente L, Reis Neto E, Neira O, Aroca Martínez G, Iglesias Gamarra A, Méndez-Patarroyo P, López R, Hernandez M, Núñez-Álvarez C, González Bello Y, Velasco Santos J, Esquivel-Valerio J, Vázquez M, Martinez de Filartiga M, Alva Linares M, Louis R, Pizzarossa C, Ralle A, Riascos M, Serventi J, Alarcon G, Pons-Estel B, Pons-Estel G. Frequency and Associated Factors of Herpes Zoster Infection in Systemic Lupus Erythematosus Patients from Latin-America [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/frequency-and-associated-factors-of-herpes-zoster-infection-in-systemic-lupus-erythematosus-patients-from-latin-america/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frequency-and-associated-factors-of-herpes-zoster-infection-in-systemic-lupus-erythematosus-patients-from-latin-america/