Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Emergency department (ED) utilization is associated with worse quality of care and health-related quality of life (HRQoL) in systemic lupus erythematosus (SLE). While frailty is a risk factor for adverse health outcomes in SLE, whether frailty is a risk factor for ED utilization in SLE is unknown. We aimed to study frailty prevalence in adults with SLE < 65 years of age compared to age- and gender-matched comparators without systemic rheumatic disease (SRD) using two validated claims-based frailty indices (CFIs) [1-2] and to assess the risk of ED utilization in frail patients with and without SLE, as well as in frail patients without SRD, compared to non-frail patients without SRD.
Methods: We conducted a longitudinal study using the Centers for Medicare and Medicaid Services Medicaid subset of the Truven Health MarketScan dataset from 2011-2016. We identified patients with SLE 18-65 years of age by ≥3 ICD-9 CM codes for SLE (710.0) ≥30 days apart during the baseline period (2011), as well as age- and gender-matched non-SRD comparators [1:4]. Baseline frailty status was determined using two CFIs validated by Segal et al. and Kim et al. [1-2]. We identified patients who were frail according to one (“frail discordant”) or both (”frail concordant”) CFIs or non-frail according to both CFIs. Agreement between CFIs was evaluated with a kappa statistic. During the follow-up period (2012-2016), we examined the risk of ED utilization in the following groups: non-frail patients without SRD (referent), non-frail with SLE, frail concordant and discordant without SRD, and frail concordant and discordant with SLE. Cox proportional hazard models were calculated, adjusting for baseline hydroxychloroquine, glucocorticoid, and immunosuppressive medication use.
Results: We identified 2262 patients with SLE and 9048 matched comparators without SRD (Table 1). Baseline frailty prevalence in patients with SLE was higher than in patients without SRD according to each CFI (Segal’s definition: 38.3% versus 21.6%; Kim’s definition: 50.4% versus 18.6%), with moderate agreement between CFIs (κ=0.47, p< 0.0001). 28.8% of patients with SLE and 11.6% of comparators without SRD were frail according to both CFIs (Table 1). Patients with SLE who were frail concordant were older and less commonly on hydroxychloroquine and immunosuppressive medication at baseline than non-frail patients with SLE (Table 1). Compared to non-frail patients without SRD, non-frail patients with SLE had a 2.1 times higher hazard of ED utilization (Table 2). Frail patients with SLE, using either frailty definition, had a 3.4 times higher hazard of ED utilization than non-frail patients without SRD (Table 2).
Conclusion: Frailty prevalence in young and mid-aged patients with SLE exceeded that in age- and gender-matched patients without SRD in this sample of Medicaid beneficiaries. Both SLE and frailty appear to be associated with a higher hazard of ED visits. Frailty may identify a subset of patients with SLE at increased risk of ED utilization and serve as a novel target for interventions to improve HRQoL in SLE.
References:
1. Segal JB et al. Med Care 2017;55:716-22.
2. Kim DH et al. J Gerontol A Biol Sci Med Sci 2018;73:980-7.
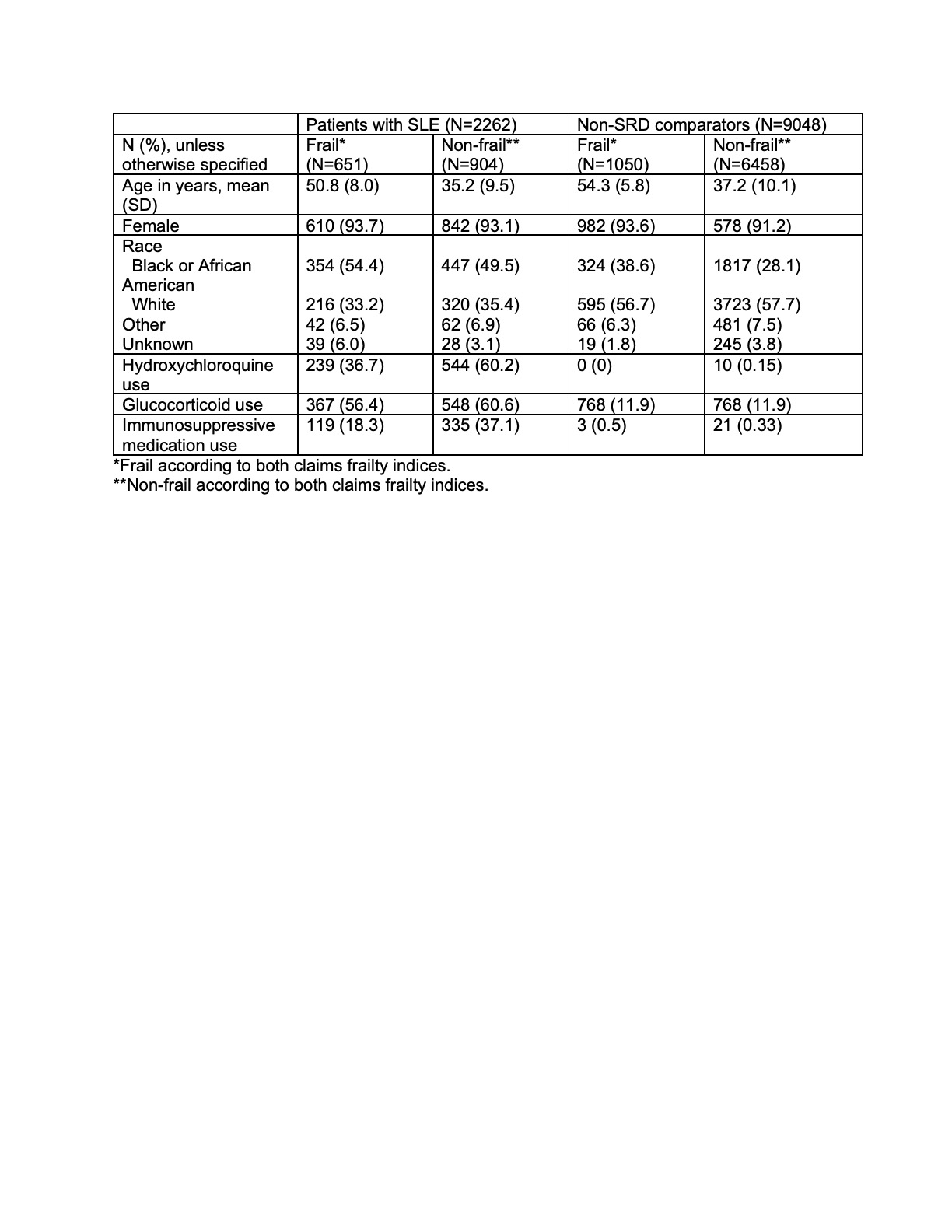 Table 1. Baseline sociodemographic features and SLE-related medication use in frail and non-frail patients with SLE and non-systemic rheumatic disease (SRD) comparators
Table 1. Baseline sociodemographic features and SLE-related medication use in frail and non-frail patients with SLE and non-systemic rheumatic disease (SRD) comparators
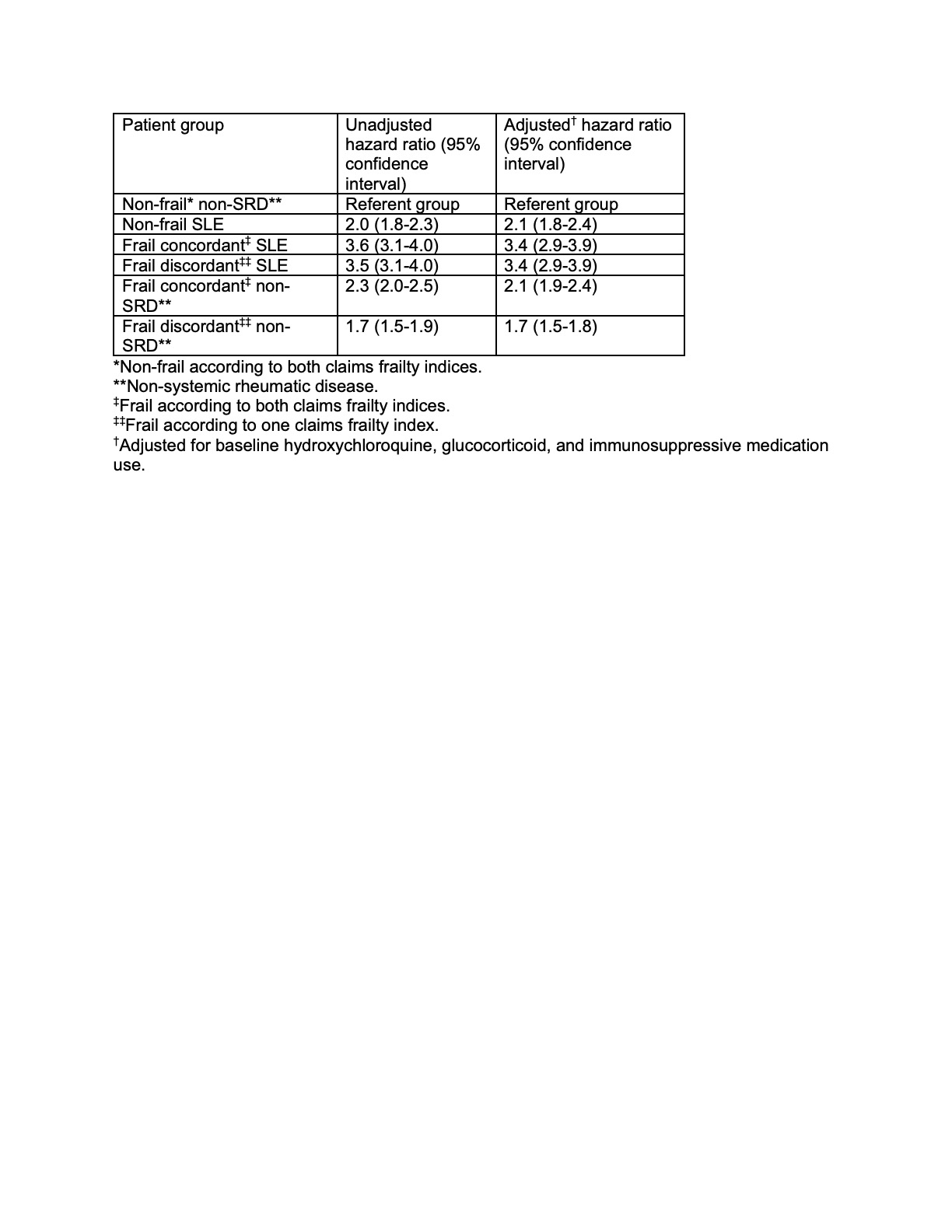 Table 2. Hazard of emergency department visits according to baseline frailty status and presence of SLE from 2011 to 2016
Table 2. Hazard of emergency department visits according to baseline frailty status and presence of SLE from 2011 to 2016
To cite this abstract in AMA style:
Lieber S, Navarro-Milln I, Nahid M, Rajan M, Sattui S, Mandl L. Frailty and Emergency Department Utilization in Systemic Lupus Erythematosus: An Administrative Claims Data Analysis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/frailty-and-emergency-department-utilization-in-systemic-lupus-erythematosus-an-administrative-claims-data-analysis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-and-emergency-department-utilization-in-systemic-lupus-erythematosus-an-administrative-claims-data-analysis/
