Session Information
Date: Monday, November 13, 2023
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders I: Imaging
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: In recent years, ultrasound has become a standard tool in the diagnosis of giant cell arteritis (GCA). Typical findings are increased intima media thickness (IMT) of the temporal and other arteries, caused by inflammation. To date, only few studies evaluated the role of ultrasound in follow-up and monitoring of GCA. 1,2 The purpose of this study was to prospectively evaluate changes of IMT of cranial and extra-cranial arteries during a 12-month follow-up of newly diagnosed GCA patients.
Methods: We prospectively enrolled patients with a new diagnosis of GCA who received glucocorticoid (GC) therapy up to seven days. Patients underwent ultrasound examinations of the axillary, carotid, vertebral, facial, and temporal arteries. IMT, total number of affected arteries, and the Omeract GCA ultrasonography score (OGUS)3, alongside laboratory parameters, current GC dose, and GCA symptoms were evaluated at baseline, after three, six, nine and 12 months. Additionally, a subgroup of patients underwent weekly exams during the first 100 days. We conducted further sub-analyses to compare ultrasound findings between patients with GCA versus GCA plus polymyalgia rheumatica (PMR), and between patients receiving GC therapy only and those receiving GC plus tocilizumab.
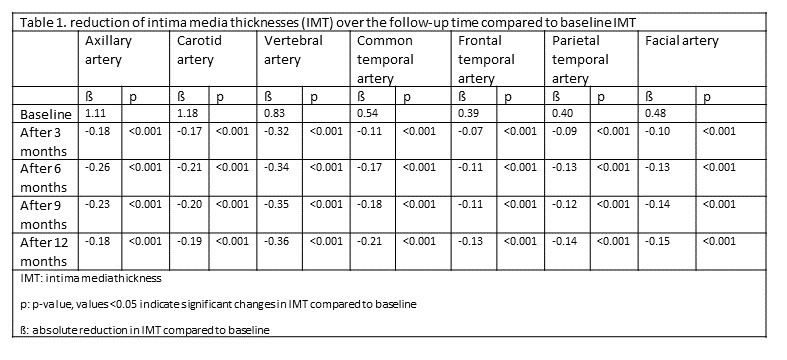
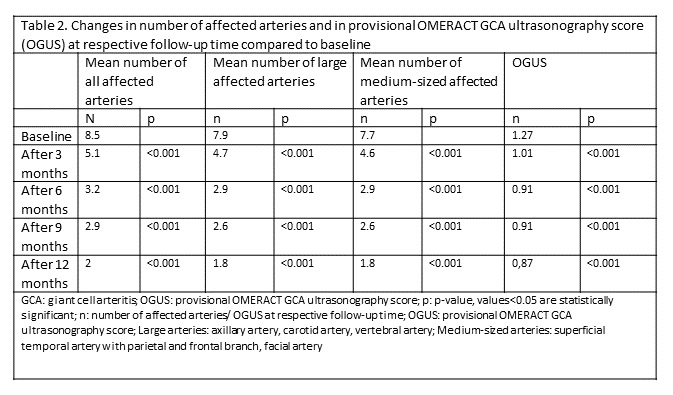
Results: Fifty patients were enrolled, 36 completed the 12-months follow-up. The cohort consisted of 23 (46%) females at a mean age of 73.6 years (SD ±8.3). The mean GC intake at baseline was 130 mg (SD ±266) at a mean of 1.7 days (SD ±2.5). In 18 patients, up to weekly exams were performed. Figure 1 displays the changes in mean IMT of all examined arteries in the first 100 days. The mean IMT of the axillary and temporal artery were normal after seven and 50 days, respectively. After six months, mean IMT of all examined arteries and OGUS were below published cut-off values.3,4,5 During the follow-up period, we observed a significant and consistent decrease in mean IMT, total number of affected arteries and OGUS (Table 1 and 2). After termination of GC therapy, follow-up visits were continued and no increase of ultrasound parameters was observed. Additionally, we found no significant differences in the reduction of these parameters between patients with GCA only and those with GCA and polymyalgia rheumatica (PMR), as well as between patients receiving GC therapy only and those receiving additional tocilizumab therapy.
Conclusion: IMT, OGUS and the total number of affected arteries decreased significantly over a 12-months follow-up period under GC with/without immunosuppressive treatment. In the first 100 days, the mean IMT of the axillary artery was found to decrease the fastest, while the mean IMT of the temporal artery was elevated for up to 50 days. Especially, the parameters did not increase after end of GC therapy. Our study underlines the important role of ultrasound examinations in monitoring of GCA.
References:
1. Bosch P et al., Therapeutic advances in musculoskeletal disease 2021; 13:1759720X21998505.
2. Ponte C et al., Ann Rheum Dis 2021; 80(11):1475–82 <
strong>3. Dejaco C et al., Ann Rheum Dis 2022.
4. Schäfer VS et al., Rheumatology (Oxford) 2017; 56(9):1479–83.
5. Ješe R et al., Rheumatology (Oxford) 2021; 60(3):1346–52.
To cite this abstract in AMA style:
Burg L, Dejaco C, Karakostas P, Behning C, Brossart P, Schäfer V. Follow-up Ultrasound Examination in Patients with Newly Diagnosed Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/follow-up-ultrasound-examination-in-patients-with-newly-diagnosed-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/follow-up-ultrasound-examination-in-patients-with-newly-diagnosed-giant-cell-arteritis/