Session Information
Date: Monday, November 6, 2017
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Disease flares in RA are associated with radiographic progression1 and functional deterioration2. Predicting flare is of direct relevance to clinical practice, particularly in patients with low disease activity (LDA) in whom treatment tapering may be considered. The aim of this study was to investigate various biomarkers as predictors of flare in patients with LDA and to evaluate the impact of flare on 12-months clinical outcomes.
Methods: The REMIRA study was a prospective cohort study in which adult RA patients on stable DMARD treatment with a DAS28 < 3.2 for > 1 month were included.3 At baseline and during every 3 months for 1 year, clinical (DAS28), functional (HAQ-DI, EQ-5D, SF36), serum (MBDA, calprotectin, CXCL10) and imaging (ultrasound) data were collected. Flare was defined as an increase in DAS28 >1.2 or >0.6 if concurrent DAS28 ³3.2 compared to baseline. Univariate Cox regression analyses were used to identify baseline predictors of flare. Subsequently, multivariate analyses were used to calculate HR for flare, adjusted for age, gender, DAS28, CRP, ESR, ultrasound and MBDA score. Linear regression analyses were performed to compare 12-months clinical outcomes between patients with and without a flare.
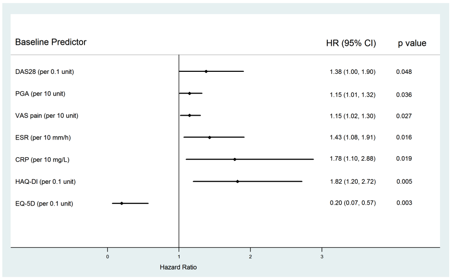
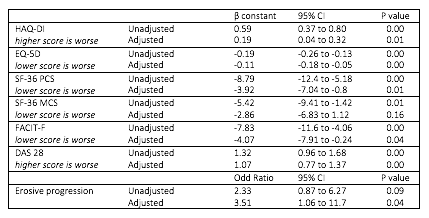
Results: In total 152 patients were included of whom 46 (30%) patients experienced a flare. Several baseline characteristics were associated with flare in univariate analyses (DAS28, ESR, CRP, PGA, HAQ-DI and EQ-5D) (Figure 1). The strongest magnitude of association was seen with HAQ-DI and EQ-5D. Baseline MBDA score, calprotectin, CXCL10 and ultrasound were not predictive of flare. A sensitivity analysis limited to flares with a rise in MBDA score to >44 (high disease activity) did show a relationship between baseline MBDA value and flare risk (1.07, 95% CI 1.02 to 1.11; p=0.005). In the multivariate analysis only HAQ-DI remained a significant independent predictor of flare (adjusted HR 1.76, 95% CI 1.05-2.93). Adjusting for baseline values, patients who flared had significantly worse clinical outcomes at month 12 (Table 1).
Conclusion: Flares occur frequently in RA patients with LDA and are associated with worse clinical outcomes after 1 year. However we found no strong predictors of flare, which may highlight a challenge in attempting to reduce flare rates or in considering patients for treatment tapering.
References: 1.Welsing PM. Arthritis Rheum 2004;50:2082Ð93.2Markusse IM. Arthritis Res Ther 2015;17:232. 3Ma M. Clin Exp Rheum April 2017
Figure 1: Univariate analyses of prediction of flare with baseline variables.
Table 1: Outcomes in flare versus no flare group
To cite this abstract in AMA style:
Bechman K, Tweehuysen L, Galloway J, Cope AP, Ma M. Flares in Patients with Rheumatoid Arthritis Are Strongly Associated with Worse Clinical Outcomes but Are Difficult to Predict [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/flares-in-patients-with-rheumatoid-arthritis-are-strongly-associated-with-worse-clinical-outcomes-but-are-difficult-to-predict/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/flares-in-patients-with-rheumatoid-arthritis-are-strongly-associated-with-worse-clinical-outcomes-but-are-difficult-to-predict/