Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Flares in PsA, presenting as periods of acute disease activity, are thought to negatively impact patients’ lives. This has not been extensively studied in a real-world setting. The objective of this study was to describe frequency of flares, assess flare impact on quality of life and work productivity, and explore predictors of flares.
Methods: A cross-sectional survey among patients with PsA recruited by rheumatologists and dermatologists was conducted in France, Germany, Italy, Spain, UK and US. Data were collected Jun-Aug 2018 via patient record forms and patient self-complete forms. Flares, by definition, could involve joints or skin or both simultaneously. Physicians recorded flare status (in flare currently/flared in last 12 months/longer than 12 months or never), demographics, physician perceived severity, and clinical outcomes. Patients reported quality of life [QoL] (EQ5D-5L), work productivity (WPAI), disability (HAQ-DI), pain (PsAID12 pain scale). Patients were compared by flare status using parametric or non-parametric tests. Logistic regression was used to explore predictors of flare. Multivariate regression was used to assess the impact of flare status on patient reported outcomes (PRO). The multivariate model was adjusted for gender, age, BMI, physician speciality.
Results: Data was collected for 2,238 patients (586 US, 1,652 EU). Mean age was 48.7 years (13.2 SD), 53.8% were male. Physicians reported 7.5% of patients were currently in flare and 22.0% had flared in the last 12 months. Patients had experienced 2.2 mean flares in the last 12 months (4.9 SD), lasting a mean 16.4 days (16.2 SD). Patients in flare were comparable demographically with those not; however, those in flare were less likely to work full time (43.6 vs. 59.3%, p< 0.01). Patients not in flare had clinically active disease (Table 1).
Results showed that flare status significantly impacted QoL, work productivity, disability, and pain (Table 2). Exploring predictors of flare in the last 12 months showed that demographic characteristics were not predictive of flare status, however patients presenting with any skin involvement or enthesitis at diagnosis were at greater risk of flare. Patients who were prescribed a bDMARD at diagnosis were at lower risk (Figure 1).
Conclusion: One third of patients surveyed were either currently in flare or had flared in the last 12 months. Being in flare adversely impacted QoL, disability and work productivity. Flare may be predicted by any degree of skin involvement or enthesitis at diagnosis.
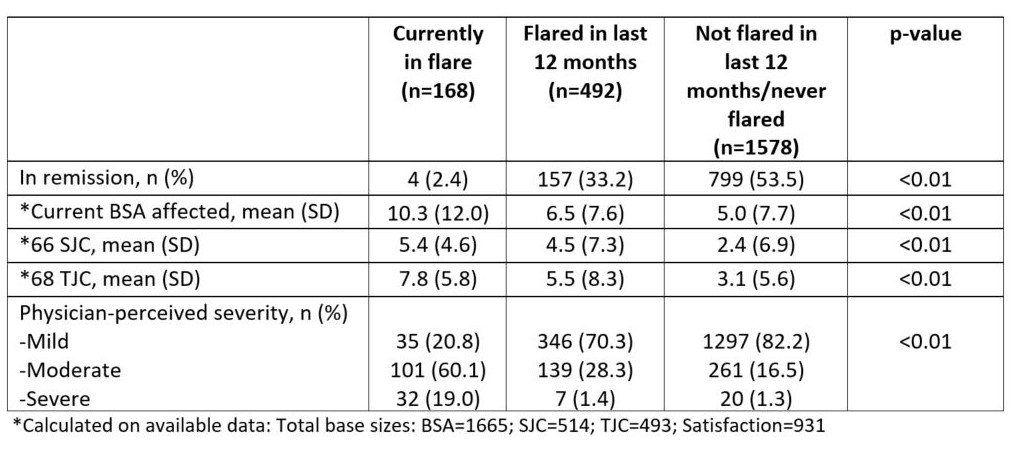 Table 1: Clinical characteristics of patients by flare status
Table 1: Clinical characteristics of patients by flare status
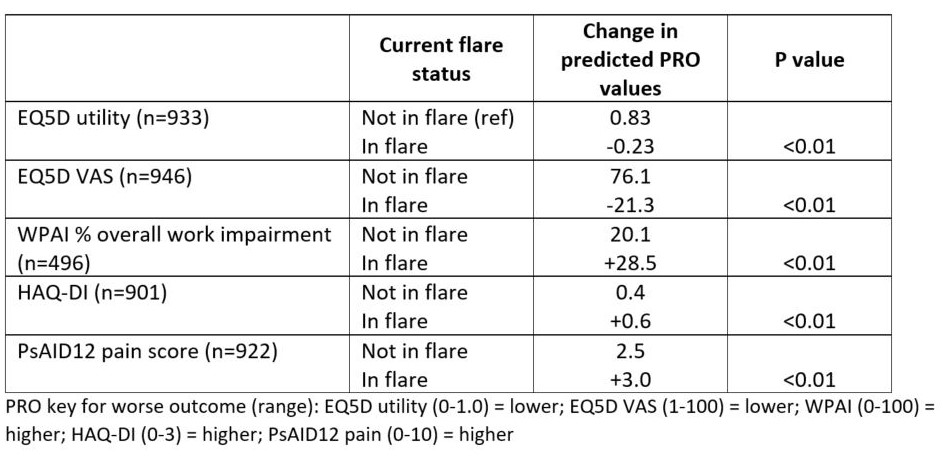 Table 2: Impact of flare status on PROs
Table 2: Impact of flare status on PROs
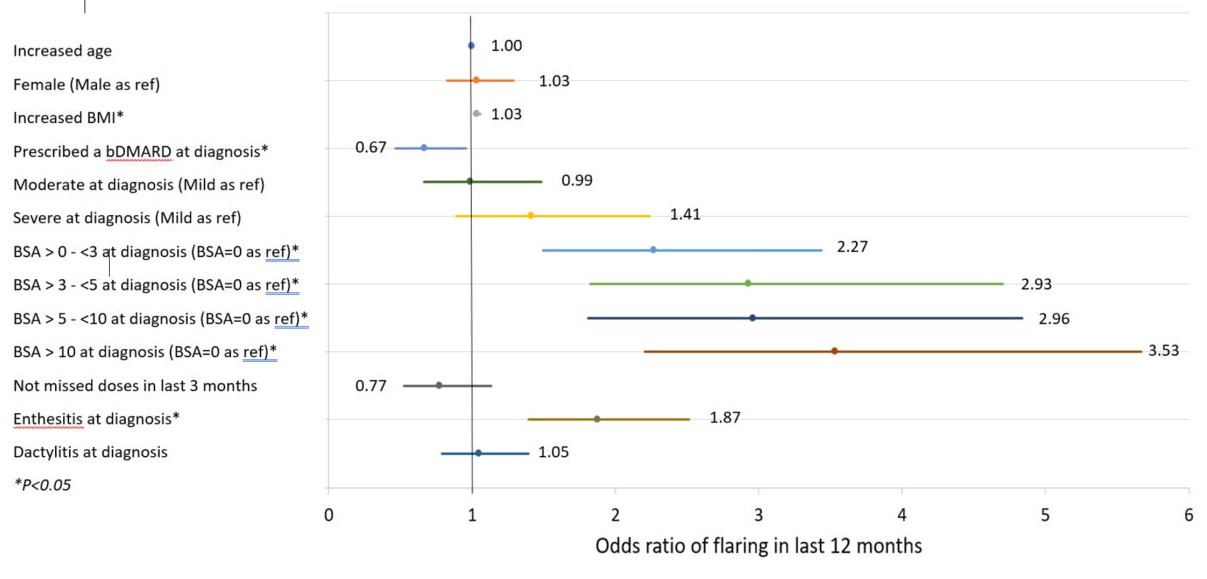 Figure 1: Predictors of flaring in last 12 months
Figure 1: Predictors of flaring in last 12 months
To cite this abstract in AMA style:
Orbai A, Tillett W, Grieb S, Piercy J, Peterson S, Holdsworth E, Meakin S, Chakravarty S, Booth N, Gossec L. Flares Among Patients with Psoriatic Arthritis (PsA) – Frequency and Impact on Patient Outcomes: Real-world Survey in the US and Europe [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/flares-among-patients-with-psoriatic-arthritis-psa-frequency-and-impact-on-patient-outcomes-real-world-survey-in-the-us-and-europe/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/flares-among-patients-with-psoriatic-arthritis-psa-frequency-and-impact-on-patient-outcomes-real-world-survey-in-the-us-and-europe/
