Session Information
Date: Sunday, November 13, 2016
Title: Pediatric Rheumatology – Clinical and Therapeutic Aspects I: Juvenile Arthritis
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Information regarding the history of patients with JIA after systemic treatment withdrawal would be helpful in driving the choice of duration therapy. While some informations in this regard exist for second-line drugs (eg methotrexate), studies on biologics are lacking. Aim of our study was to assess the time on remission after discontinuing biologic therapy in a retrospective, comparative, multicenter, cohort study of patients with JIA,
Methods: Among 349 JIA patients followed in three tertiary care centres and treated with biologics (started before age 18 y), 135 (103 F, 32 M; median age 15 years) achieved remission and could discontinue such treatment. Only first cycle of biologics was considered for this study: 87 received Etanercept, 27 Adalimumab, 12 Infliximab, 7 Anakinra, 1 Rituximab, and 1 Abatacept. Primary outcome was to assess, once remission was achieved, the time on remission up to the first flare after discontinuing treatment. Time to achieve remission once biologic drug was started, corticosteroid usage, and time on remission on therapy before discontinuing all treatments were also considered, along with demographic, clinical, and laboratory data. Mann–Whitney U-test, Wilcoxon signed-rank test for paired samples, chi-square, and FisherÕs exact test, when appropriate, were used to compare data. Pearson and Spearman correlation tests were used to determine correlation coefficients for different variables. In order to identify predictors of outcome Cox regression model and Kaplan–Meier curves were constructed, each one at mean of entered covariates.
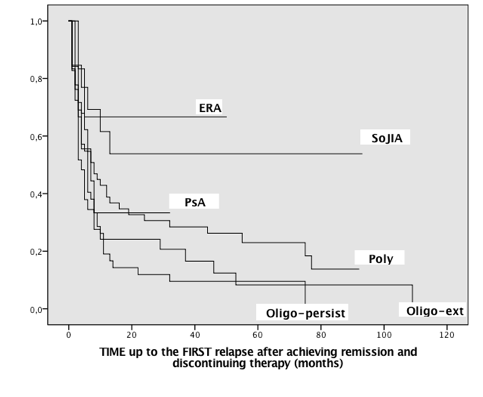
Results: The vast majority of enrolled patients flared after stopping treatment with biologics (102/135, 75.6%) with a median follow-up time on remission of 6 months (range 1–109) [Figure1]. Considering the time point one year after treatment discontinuation 43/135 (31.9%) patients were still in remission. For this group, remission lasted for a median period of 53 months (range 12-109): 30/48 with polyarticular onset, 7/27 oligoarticular extended, 6/35 oligoarticular persistent, 2/6 enthesitis-related arthritis (ERA), 2/7 psoriatic arthritis, and 8/12 systemic onset JIA. A higher probability of maintaining remission after discontinuing treatment was present in systemic onset disease and in ERA compared to the rest of JIA patients (Mantel-Cox χ2 14.58, p<0.012) [Figure 2]. ANA positivity was associated with a higher probability of flare (Mantel-Cox χ2 4.17, p<0.04). Patients who received biologics > 2 years after achieving remission had a higher probability of maintaining such remission off therapy (median 21.74 ±3.4 months vs 13.4 ±2.3; Mantel-Cox χ2 6.86, p<0.009). No other clinical variable, including total length of treatment and type of treatment, resulted significantly associated with a long-lasting remission.
Conclusion: Even if in a retrospective study, we showed that patients with ANA positivity and those who stop treatment before two years of remission have a higher chance of relapsing after biologic withdrawal, and that patients with systemic onset disease and ERA are less likely to flare. 
To cite this abstract in AMA style:
Simonini G, Scoccimarro E, Pontikaki I, Ferrara G, Giani T, Taddio A, Meroni PL, Cimaz R. Flares after Withdrawal of Biotherapies in JIA: Clinical and Laboratory Correlates of Remission Duration [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/flares-after-withdrawal-of-biotherapies-in-jia-clinical-and-laboratory-correlates-of-remission-duration/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/flares-after-withdrawal-of-biotherapies-in-jia-clinical-and-laboratory-correlates-of-remission-duration/