Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Manifestations of SLE are known to affect patient-reported outcome measures (PROs) such as physical function, fatigue, and pain. Other work has suggested economic insecurity is associated with worse PRO scores, and discrimination can have a chronic effect on health status. This study focused on the association of PROs with individual and structural socioeconomic factors and SLE-related clinical variables.
Methods: A cohort of patients (n=272) diagnosed with SLE according to standard classification criteria (ACR revised classification, European Alliance of Association for Rheumatology/ACR classification, or SLICC classification) were surveyed using measures from the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) for physical function, cognitive function, pain interference, fatigue, anxiety, sleep disturbance, and depression. Analyses included demographics, financial/material insecurity such as in housing, finances, healthcare, or job status, and clinical data on disease activity (any of cutaneous, nephritis or arthritis) and immunosuppressive medication use. Everyday Discrimination Scale was captured to quantify the potential impact of discrimination and its associated chronic stress on health (coded as never vs ever experienced 9 discrimination types and summed across types). Multivariable linear regression models of PROs included clinical and socioeconomic factors.
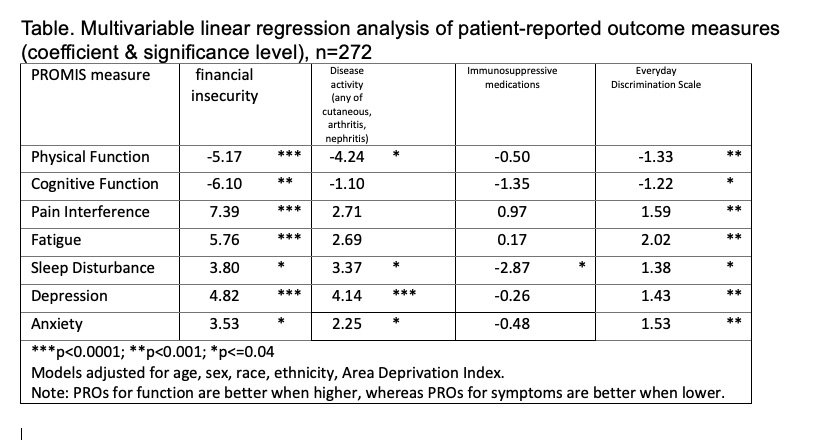
Results: The cohort was 90% female, 28% African American/Black, 17% Asian, 39% white, and 16% other/unknown, with an average age of 40 years. Average SLEDAI was 3.17 (SD=3.52) and SLICC damage score 1.12 (SD=1.53). Multivariable models showed that experiencing financial insecurity was associated with significantly worse scores on all PROs, from 4-7 points worse (p< 0.01). Each additional point on the Everyday Discrimination Scale was associated significantly with 1 point worse on physical and cognitive function score, 1 point higher sleep disturbance, depression, and anxiety, and 2 points higher on fatigue on average (p< 0.05). Finally, experiencing disease activity was significantly associated with lower physical function and higher sleep disturbance, depression, and anxiety (p< 0.05). (Table)
Conclusion: Experiencing financial insecurity was associated with clinically important negative impacts in function and symptom PROs; everyday discrimination consistently significantly negatively affected PRO scores; and disease activity was negatively associated with 4 of the 7 measures. Understanding the full experience of patients with SLE, beyond their clinical manifestations, may help identify approaches to support patients for improved function and reduced symtpoms.
To cite this abstract in AMA style:
Gold H, Li Y, Izmirly P, Buyon J, Masson M, Saxena A, Belmont H, Tseng C, Anthopolos R. Financial insecurity and discrimination are associated with patient-reported quality of life in patients with SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/financial-insecurity-and-discrimination-are-associated-with-patient-reported-quality-of-life-in-patients-with-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/financial-insecurity-and-discrimination-are-associated-with-patient-reported-quality-of-life-in-patients-with-sle/