Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Pain research conceptualizes fibromyalgia (FM) as a Physical or Somatic Symptom Disorder (PSD or SSD). However, the 2013 Diagnostic and Statistical Manual of Mental Disorders (DSM-5) identifies an SSD mental disorder (DSM-SSD) when there are findings of “positive symptoms (distressing somatic symptoms + excessive thoughts, feelings, and behaviors in response to these symptoms),” whether or not the symptoms are “medically explained.” FM is defined on the basis of somatic symptoms and concerns arose that DSM criteria would turn FM into a mental disease. We examined DSM mental illness in patients with rheumatoid arthritis (RA), including those with FM. We utilized RA patients to provide a large subject base and appropriate control subjects, and to avoid self-selection for severity.
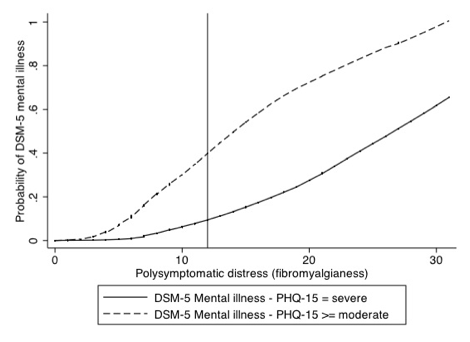
Methods: We used the Patient Health Questionnaire-15 (PHQ-15), a validated assessment of somatic symptom severity, to operationalize the DMS-5 SSD definition. For mental illness Definition 1 a DSM-SSD positive individual had to have at least 2 “severe” symptoms (“bothered a lot”) and a total PHQ-15 somatic symptom severity classification of “medium” (10-14) or “high” (>=15). A second, more restrictive definition (Definition 2) required the total PHQ-15 symptom severity classification to be high (>=15). We diagnosed FM according to the survey modified 2010 FM criteria.
Results: Of the 4718 RA patients, 22.1% were definition 1 DSM-SSD positive and 6.7% definition 2 positive (Table 1). When FM (+) patients were considered, 68.8% and 28.8% satisfied mental illness 1 and 2 definitions. 19.8% of RA patients also satisfied ACR2010 criteria. The probability of satisfying the mental illness definitions increased as a function of polysymptomatic distress (fibromyalgianess) (Figure 1). Persons who met either definition had more abnormal scores for all severity and outcome measures, including functional status, pain, quality of life, household income, etc.
Conclusion: There are serious problems of face validity when mental illness is defined on the basis of “excessive thoughts, feelings, and behaviors” in response to somatic symptoms, as somatic symptoms form the basis of rheumatic diseases. In addition, somatic symptoms increase in number and severity with increasing pain, and no clear direction of causality can be discerned. If somatic symptoms are to be expected in rheumatic diseases, then it all comes down to “excessive”, a term that cannot be reliably or validity defined. The high rates mental illness identified by the DSM-SSD definition in our study suggest the mental illness classification is invalid.
|
|
FM (-) (80.2 %) |
FM (+) (19.8 %) |
All |
|
Mental illness 1 (%) |
10.7 |
68.8 |
22.1 |
|
Mental illness 2 (%) |
1.2 |
28.8 |
6.7 |
|
PHQ-15 |
5.6 |
12.3 |
6.9 |
|
Polysymptomatic distress |
63.0 |
19.3 |
8.7 |
Disclosure:
F. Wolfe,
None;
B. T. Walitt,
None;
R. S. Katz,
None;
W. Häuser,
Pfizer Inc,
5,
Daiichi Pharmaceutical Corporation,
5,
Abbott Laboratories,
5.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fibromyalgia-somatic-symptoms-and-mental-illness-in-view-of-the-2013-diagnostic-and-statistical-manual-of-mental-disorders/