Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
Fibromyalgia (FM) is a condition characterized by chronic widespread pain, tender points, fatigue and disturbed sleep rhythm. Some of these symptoms such as fatigue, tender points and diffuse pain seen in patients with spondylarthritis (SpA). Moreover, FM and SpA can coexist creating a diagnostic challenge, particularly in early disease course and influence clinical disease activity assessment. With this cross-sectional study, we aim to estimate the prevalence of FM in SpA and to elaborate its effect on biological treatments.
Methods: FM was identified according to the ACR 2010 diagnostic criteria. SpA patients identified according to rheumatologist using various SpA subsets criteria. A review of the electronic medical files for SpA patients attending the rheumatology outpatient clinic and infusion unit at a major tertiary hospital during the period from June to December 2018 were included. Patients’ demographics, disease characteristics were explored. Regarding SpA medications, number, frequency and dose of DMARDs and biological agents were obtained. Continuous variables were reported by their mean and standard deviation (SD) and qualitative variables by frequency and percentage. Statistical significance was set at p < 0.05. Statistical analysis was performed using SPSS version 23.
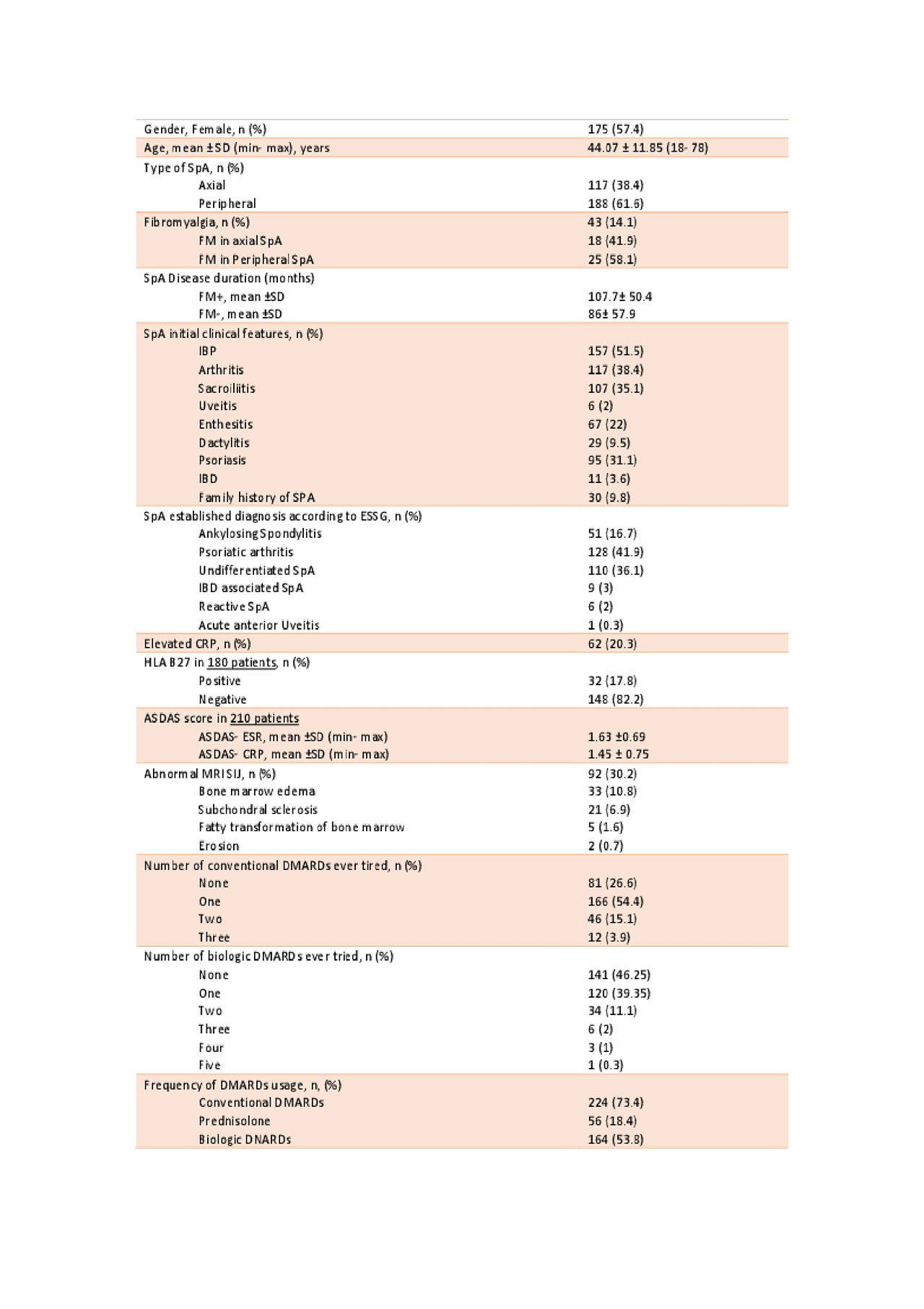
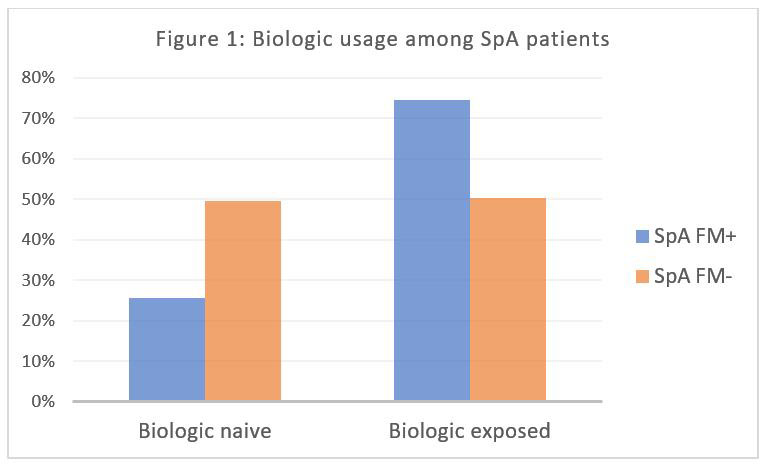
Results: Of the 305 enrolled SpA patients, 43 (14.1%) had FM. Females represents 57.4% of the patients, mean age was 44.07 ± 11.85 years. Arab ethnicity represents most of our cohort 84.9%, the majority were Emirati 64.6%. Smokers were 8.2% and ex-smokers were 3.3%. HLA B27 tested in a sample of 180 patients; it was positive in only 17.8%. Abnormal MRI SIJ bone marrow edema changes were found in 10.8%, while other SIJ changes was seen in additional 20.6%. The prevalence of FM showed no statistically significant difference between axial and peripheral SpA. Patients with SpA and FM have longer disease duration than SpA alone, P= 0.034. Table.1 show demographics and clinical data. Regarding medication, the use of biologics in SpA patients with FM is more frequent than SpA patients without FM (74.4% vs 51.5 % respectively), P= 0.005 (Figure: 1). Interestingly, the likelihood ratio testing showed that SpA patient with Fibromyalgia switch more frequently to another biologics, P= 0.015 (Figure: 2). Cramer’s V test showed that there is a high statistically significant (P= 0.002) and very strong association ( > 0.25) between presence of Fibromyalgia and multiple switching of biologics in SpA. There was no difference in the exposure to prednisolone nor conventional DMARDs between SpA patients with or without FM, P= 0.64 & 1 respectively.
Conclusion:
FM coexistence with SpA might impact clinical evaluation of disease activity and negatively affect measures of treatment response. In our study, SPA patients exposed to more biologics if they have coexisting FM; Moreover, they are more frequent switchers among biologics including TNFi and IL17i.
To cite this abstract in AMA style:
Negm A, Elsidig N, Al Marzooqi A, Zamani N, Hossaini A, Al Saleh J. Fibromyalgia and Multiple Switching of Biologics in Spondylarthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/fibromyalgia-and-multiple-switching-of-biologics-in-spondylarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/fibromyalgia-and-multiple-switching-of-biologics-in-spondylarthritis/