Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: JIA studies demonstrate that there is a “window of opportunity” early in the disease course during which appropriate management improves outcomes: prompt referral to pediatric rheumatology (PR) center is crucial for best results. There are no publications about patient’s pathway until first PR visit from India. In this country, the number of JIA is huge: the estimated prevalence ranges from 350 000 to 1.3 million. Health-care costs are paid out of pocket by patients and there is a significant shortage of pediatric rheumatologists (PRsts) with approximately 15 PRst concentrated in urban centres. These parameters are likely to impact referral pathways. This study aimed to describe time from onset of symptoms to first PR visit of JIA patients to a tertiary center in India and to analyze predictive factors for time to referral.
Methods: This retrospective study is from data collected on JIA patients in the PR center, Institute of Child health, Sir Ganga Ram Hospital (SGRH) in New Delhi where both paid (private) and free (poor) patients are seen. JIA patients fulfilling ILAR 2004 criteria and seen at least twice from 01/10/2013 to 30/09/2018 were included. Data collected were: demographic details, history of the disease, referral practitioner, clinical and laboratory features, treatment. Patients previously assessed by PRst or with missing data were excluded. Mann-Whitney U-test, Chi square and logistic regression (univariate and multivariate) were used as appropriate to study factors that determined time to first PR visit.
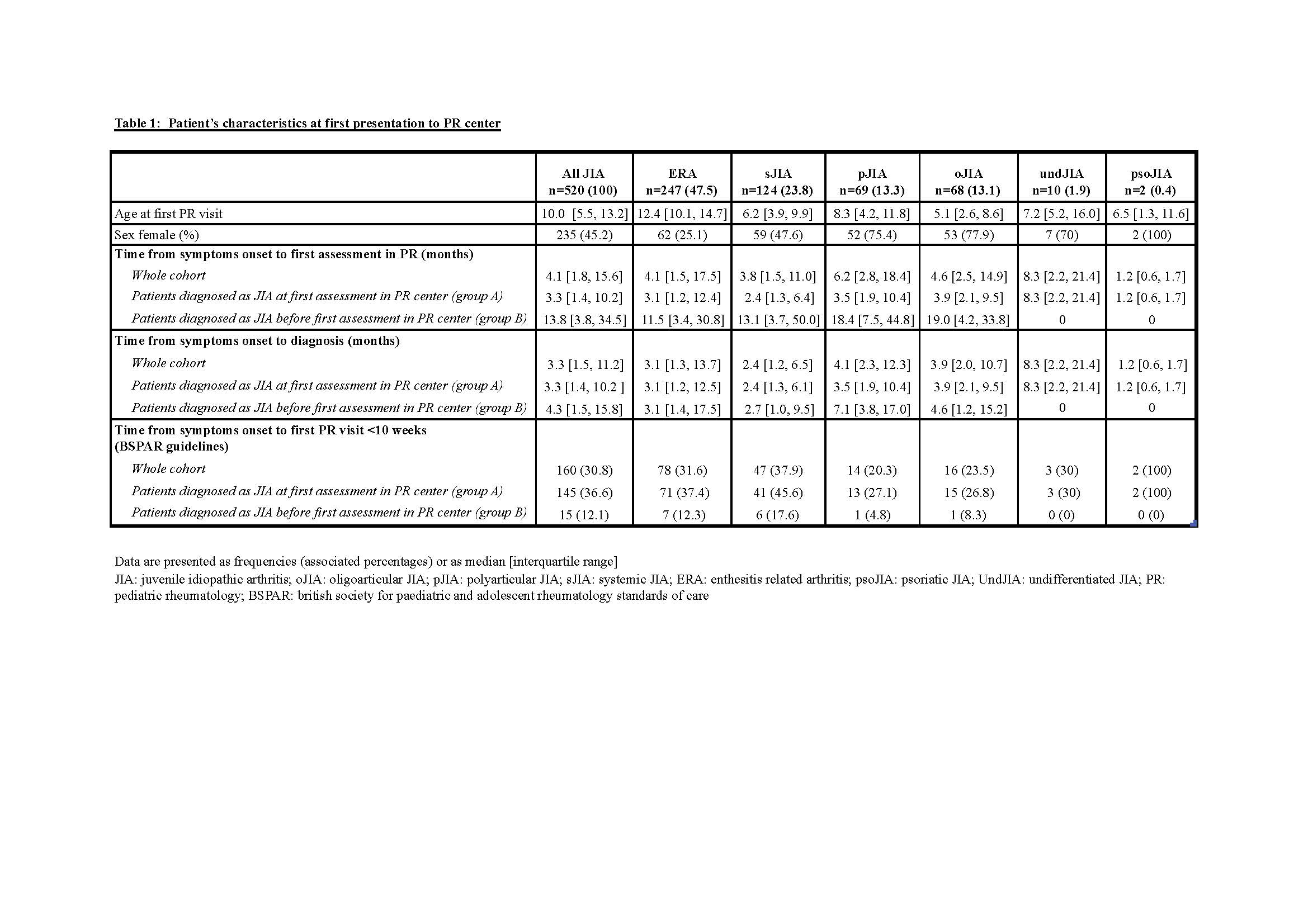
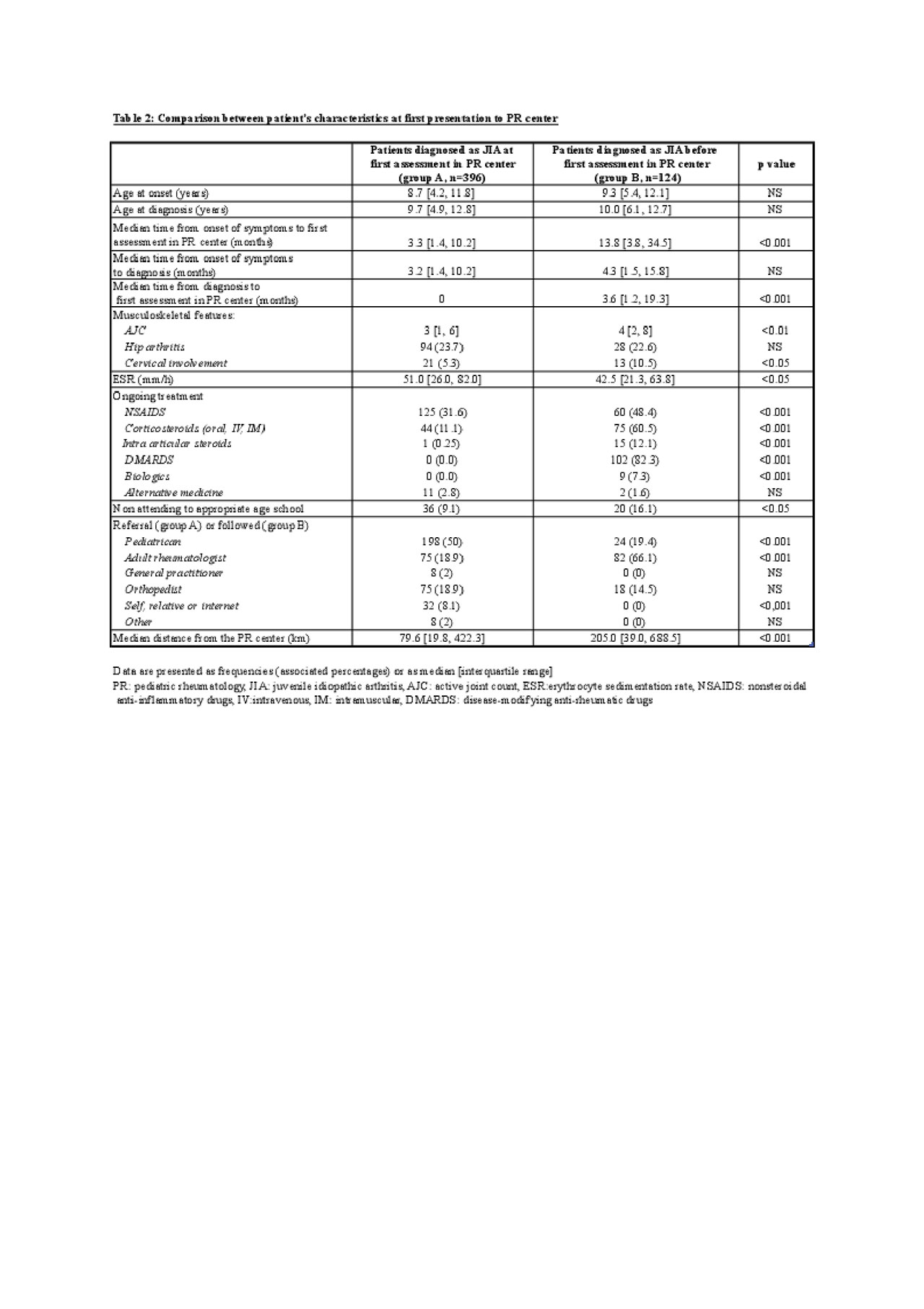
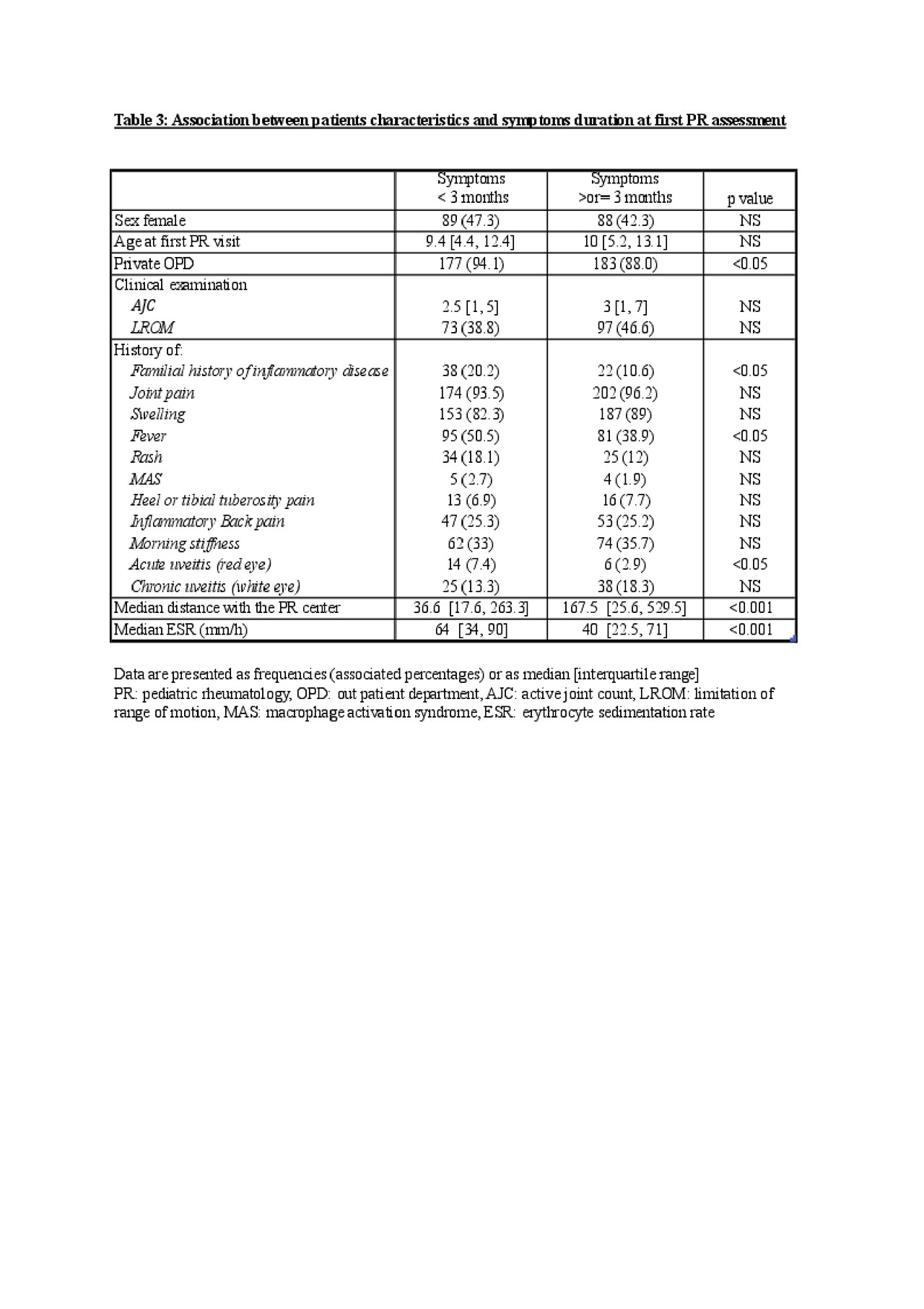
Results: In all 520 patients were included (45% girls, median age 10 years, 71% were systemic JIA patients and enthesitis related arthritis patients (table 1)): 396 children were diagnosed at our PR center (group A), 124 were previously diagnosed as JIA and managed by non PRst before first PR visit (group B). Median time of symptom onset to first assessment in PR was 4.1 months and median distance travelled 119.5 km. Despite ongoing treatment at first PR visit, group B patients had more aggressive disease (active joint count 4 versus 3, p< 0.01; cervical involvement 10.5% versus 5.3 %, p< 0.05; children non attending to school 16.1% versus 9.1%, p< 0.05) and resided further away (205 km versus 79.6 km, p< 0.001). For group B patients, predominant referral doctor was adult rheumatologist (66%), for group A- pediatrician (50%) (table 2). On univariate analysis, factors that predicted PRst visit within 3 months were private patients, short distance to travel, family history of inflammatory disease, history of fever, history of acute uveitis or high ESR. On multivariate analysis all factors remained except high ESR.
Conclusion: Time to first PR assessment at this center is comparable to western countries(1). Cost of care and long distance to travel were factors that delayed consultation ; acuity of complaints, short distance to travel, adequate financial resources and a family member with rheumatologic condition hastened referral.
Possible factors to improve referral to PR centres would be to increase the number of PRst and to provide free medical insurance countrywide. Indeed many families can ill afford the travel and cost of care for a child with JIA.
- McErlane F et al. Rheumatology (Oxford). 2016 Jul
To cite this abstract in AMA style:
Freychet C, Agarwal M, Mittal S, Shivpuri A, Singh A, Dinand V, Sawhney S. Factors Impacting Referral of Juvenile Idiopathic Arthritis Patients to a Tertiary Level Pediatric Rheumatology Center in North India [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/factors-impacting-referral-of-juvenile-idiopathic-arthritis-patients-to-a-tertiary-level-pediatric-rheumatology-center-in-north-india/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-impacting-referral-of-juvenile-idiopathic-arthritis-patients-to-a-tertiary-level-pediatric-rheumatology-center-in-north-india/