Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Patients and physicians often perceive the extent of disease activity differently. We aimed to assess the factors contributing to the variability in scoring of patient global assessment (PGA), physician (assessor) global assessment (AGA) of disease activity and the discrepancy in scoring between PGA and AGA among patients with psoriatic arthritis (PsA).
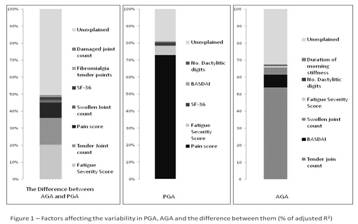
Methods: A cross sectional study was conducted of patients attending a large PsA clinic from 2008 to 2013. Three different outcomes were studied: AGA, PGA and the difference between AGA and PGA. The scores of PGA and AGA ranged from 0 (no disease activity) to 10 (high disease activity). The difference between AGA and PGA reflected the discrepancy between the physician and patient global assessment of joint activity and could take values from -10 (worse estimation of disease activity by the patient) to 10 (worse estimation of disease activity by the physician). Predictors of these outcomes included demographics, skin and joint assessment by the physician, patient reported information about function, quality of life and fatigue. Multivariate linear regression identified variables that contributed significantly to each of the outcomes. The proportion of variability of each outcome explained by each predictor was expressed using a partial R2.
Results: A total of 565 patients were included in the analysis. Their mean age was 51.7±13.2 years and 58.6% were males. The mean duration of psoriasis and PsA were 24±13.8 and 14.3±19.4 years, respectively. 81% of the variability in PGA and 68% of the variability in AGA were explainable. The main factors associated with PGA were pain (R2partial =72.9%, Figure 1), fatigue (by Fatigue Severity Scale (FSS) R2partial =5.5%) and disability scores (by Short Form (SF) -36 R2partial =2.1%). The main factors associated with AGA were tender joint count (R2partial =53.9%), swollen joint count (R2partial =4.2%) and patient perception of joint activity (by Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) R2partial =7.5%). Increased fatigue by FSS accounted for 20.4% of the variation in the difference between AGA and PGA and pain (R2partial =9.2%) and disability scores by SF-36 (R2partial =1.6%) were also important; these led to worse patient assessments while increased tender joint count (R2partial =15.9%) and swollen joint counts (R2partial =1.7%) resulted in a worse physician assessment of arthritis.
Conclusion: Fatigue, pain, disability, tender and swollen joint counts were the most important factors contributing to discrepancy between patient and physician assessment of joint activity.
Disclosure:
L. Eder,
None;
A. Thavaneswaran,
None;
V. Chandran,
None;
R. J. Cook,
None;
D. D. Gladman,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-explaining-the-discrepancy-between-patient-and-physician-global-assessment-of-disease-activity-in-psoriatic-arthritis/