Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Takayasu arteritis (TAK) is an inflammatory disease which primarily affects large vessels. However, as a systemic disease, the spectrum of its manifestations is not limited to the arterial wall.
Methods: Data records of TAK patients diagnosed according to the 1990 ACR criteria and followed-up at our Large Vessel Vasculitis Clinic were reviewed. Any significant inflammatory/autoimmune comorbidity and family history for inflammatory/autoimmune disease were considered. For each comorbidity, temporal correlation with TAK diagnosis was assessed. Need for biological therapy for TAK control, as an indirect measure of TAK aggressiveness, was evaluated. Non-parametric statistic tests were used.
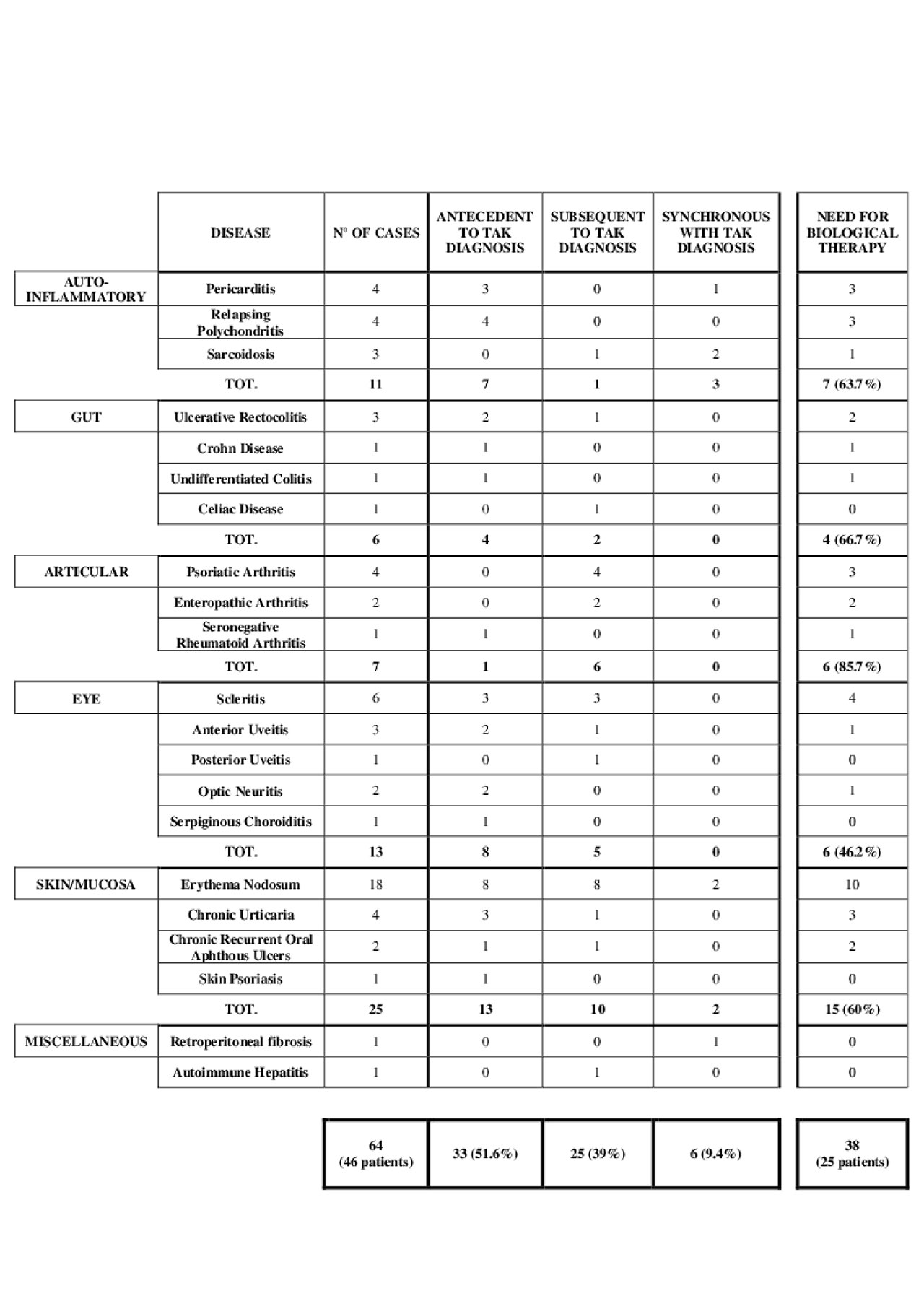
Results: In our cohort of 128 TAK patients, 46 patients (35.9%) were identified as having an inflammatory/autoimmune comorbidity, for a total of 64 comorbidities (14 patients experienced >1 comorbidity). Comorbidities were classified into 6 categories: systemic inflammatory diseases (11 patients, 14.3%); gastro-intestinal (6 patients, 7.8%), articular (7 patients, 9.1%), ocular (13 patients, 16.9%) and muco-cutaneous (25 patients, 32.5%) involvement; miscellaneous (autoimmune hepatitis, retroperitoneal fibrosis). In 33 cases (51.6%) the comorbidity onset preceded, in 25 (39%) followed and in 6 (9.4%) was synchronous with TAK diagnosis (Table 1). In 25 patients (54.3%) use of a biological therapy to control TAK activity was needed (versus 35.4% in TAK patients without comorbidities, p = 0.042). Having a comorbidity increased the risk for the introduction of a biologic therapy, odds ratio=2.176 (1.042-4.541). Of the 128 TAK patients, 17 (13.3%) had a positive family history for inflammatory or autoimmune diseases (8 psoriasis, 5 rheumatoid arthritis, 3 inflammatory bowel disease, 1 sarcoidosis).
Conclusion: In TAK patients, extravascular involvement is a common finding and usually precedes the vascular involvement (the only significant exception is represented by inflammatory arthritis). Inflammatory and autoimmune extravascular comorbidities seem to be associated with a significant higher burden of vascular inflammation, as inferred by the higher rate of biological therapies use in these TAK patients.
To cite this abstract in AMA style:
Baldissera E, Tomelleri A, Sartorelli S, Campochiaro C, Dagna L. Extravascular Inflammatory Manifestations of Takayasu Arteritis in a Monocentric Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/extravascular-inflammatory-manifestations-of-takayasu-arteritis-in-a-monocentric-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/extravascular-inflammatory-manifestations-of-takayasu-arteritis-in-a-monocentric-cohort/