Session Information
Date: Monday, November 9, 2015
Title: Rheumatoid Arthritis - Clinical Aspects III - Cardiovascular Disease and RA
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Several recent studies have
identified RA patients with very low levels of circulating total and low
density lipoprotein cholesterol (LDL-C) to be at particularly high risk for
cardiovascular disease (CVD) events. However, it is unknown whether coronary
atherosclerosis is higher than expected among those with low lipid levels.
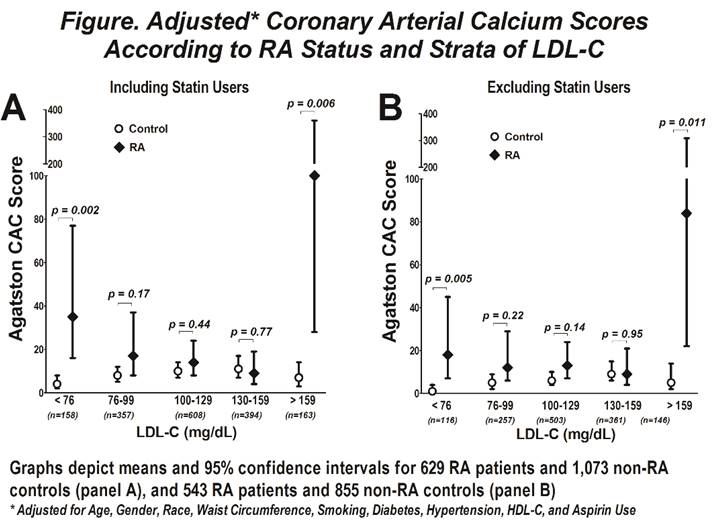
Methods: Data were pooled from 4 U.S. cohorts of RA
patients and a compatible cohort of non-RA controls who all underwent similar
assessments of serum lipids and coronary atherosclerosis [cardiac computed
tomography scanning with coronary arterial calcium (CAC) calculated using the
Agatston method]. Patients with prior known CVD were excluded. CAC scores
according to strata of serum lipids were compared between the RA and control
groups using multivariable (MV) linear regression, adjusting for pertinent
confounders. The lowest stratum of LDL-C was defined at<76 mg/dL. Analyses
were repeated excluding lipid lowering medication (LLM) users.
Results: A total of 629 RA patients and 1,073 non-RA
controls were studied. Adjusting for unbalanced demographics, on average, the
RA group had significantly lower BMI and waist circumference, higher systolic
and diastolic blood pressures, more NSAID use and less use of aspirin.
Smoking, diabetes, and HDL-C were similar between the groups. Mean total cholesterol
did not differ for RA vs. control (193 vs 194 mg/dL, respectively; p=0.73);
however, mean LDL-C was lower in the RA group (114 vs. 118 mg/dL; p=0.031). A
higher proportion of RA patients had LDL-C<76 mg/dL (13 vs 8%; p=0.004), even
when excluding LLM users (11 vs 7%; p=0.023). Adjusting for demographics,
moderate/severe CAC (i.e. CAC≥100 units) was observed in 30% of the RA
group compared with only 18% of controls (p<0.001).
In controls, the lowest average adjusted CAC
scores were observed in those with a LDL-C<76 mg/dL. In contrast, average
CAC scores were nearly 9-fold higher for RA patients in the same LDL stratum
(p=0.002; Panel A). Absolute differences between the groups were diminished
after excluding LLM users; however, RA patients with the lowest and highest
LDL-C levels still had significantly higher CAC compared with controls.
Similar relationships were observed for strata of total cholesterol. RA
patients with LDL-C<76 mg/dL and not taking LLM were less likely to be RF
positive and more likely to be prescribed hydroxychloroquine compared with
those with higher LDL-C. They did not differ on disease duration, disease
activity measures, or treatment with other DMARDs or prednisone.
Conclusion: These data suggest that RA patients with
very low LDL-C may be candidates for heightened CVD screening and prevention
To cite this abstract in AMA style:
Giles JT, Wasko MCM, Chung CP, Kao A, Bokhari S, Zartoshti A, Stein CM, Bathon JM. Exploring the Lipid Paradox Theory in Rheumatoid Arthritis: Subclinical Coronary Atherosclerosis Is Higher Among Rheumatoid Arthritis Patients with the Lowest Circulating Low Density Lipoprotein Concentrations Compared with Controls [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/exploring-the-lipid-paradox-theory-in-rheumatoid-arthritis-subclinical-coronary-atherosclerosis-is-higher-among-rheumatoid-arthritis-patients-with-the-lowest-circulating-low-density-lipoprotein-conce/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploring-the-lipid-paradox-theory-in-rheumatoid-arthritis-subclinical-coronary-atherosclerosis-is-higher-among-rheumatoid-arthritis-patients-with-the-lowest-circulating-low-density-lipoprotein-conce/