Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Subclinical inflammatory lesions detected by MRI are prevalent in hand joints of patients with cutaneous psoriasis (1). Yet, it is unknown whether these inflammatory changes persist in patients with psoriatic arthritis (PsA) in low disease activity/clinical remission. Minimal disease activity (MDA) is a validated composite index used for clinical evaluation in PsA(2). The purpose of this study is to estimate the prevalence of hand inflammatory changes in PsA patients with MDA versus non-MDA (active disease) using MRI.
Methods: Sixty consecutive prospectively recruited patients with peripheral PsA (CASPAR criteria) underwent clinical evaluation, questionnaires, and MRI of a predominantly involved hand within 72 hours of the clinical examination. MRI scans were scored for synovitis, tenosynovitis, periarticular inflammation, bone edema, bone erosion, and bone proliferation according to the OMERACT PsA MRI scoring system (PsAMRIS) method(3), performed by an expert musculoskeletal radiologist, blinded for clinical data.
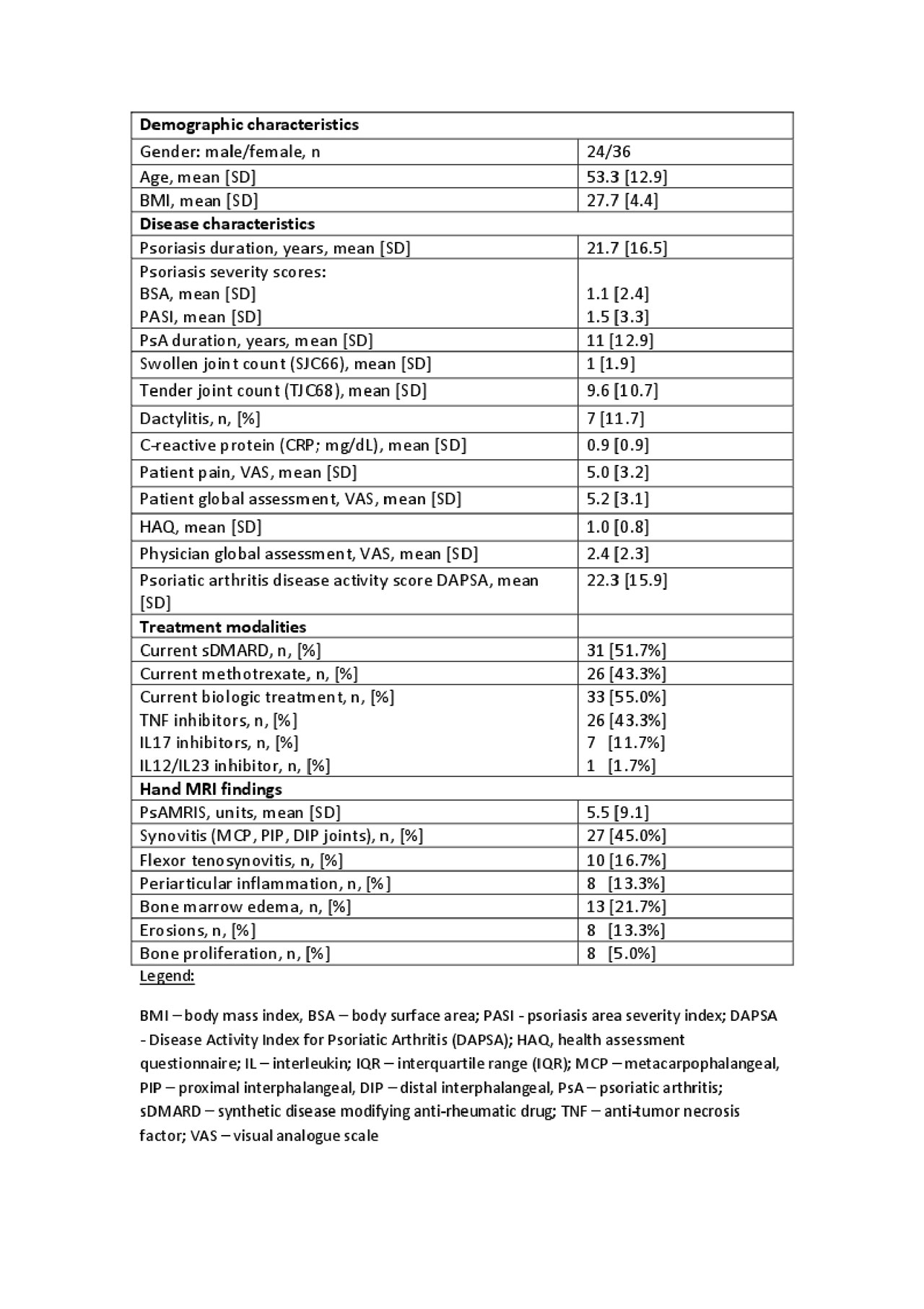
Results: Clinical characteristics of the PsA cohort and prevalence of hand MRI lesions are presented in Table 1. The mean total PsAMRIS of the cohort was low (5.5 units [SD 9.1]), with synovitis of MCP joints being the most common finding (n=27 patients, [45%]). PsA duration was moderately correlated with the total PsAMRIS (Spearman’s rank correlation rho 0.358, p=0.005).
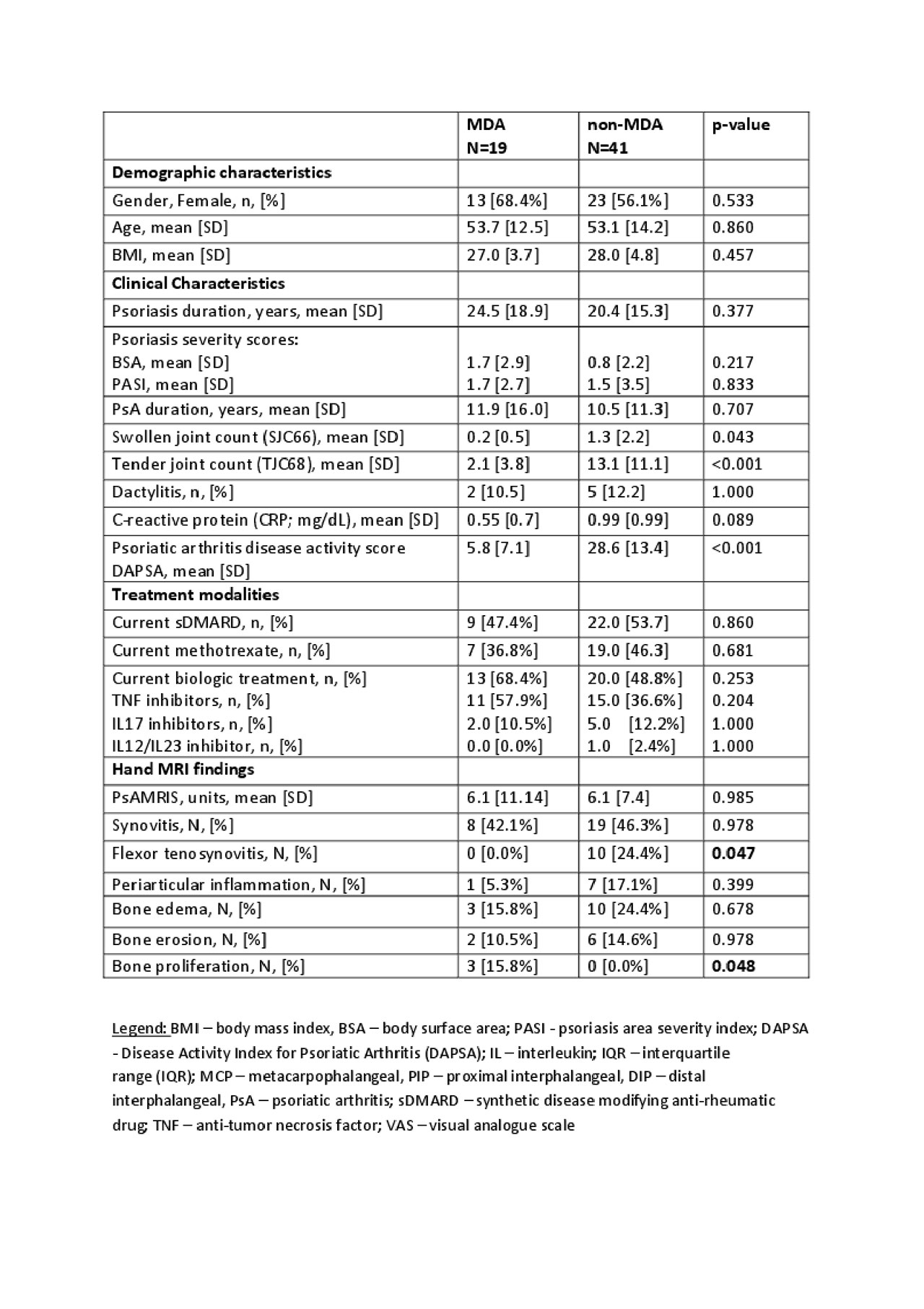
MDA (n=19) and non-MDA (n=41) groups were comparable in age, BMI, psoriasis/PsA duration, skin disease severity, and treatment modalities. (Table 2) Total PsAMRIS units (mean [SD]) was similar in MDA and non-MDA groups: 6.1 [11.14] vs 6.1 [7.4], respectively (p=0.985). Remarkably, both groups had a similar prevalence of hand synovitis with predominant involvement of MCP joints: MDA vs non-MDA, n=8 [42.1%] vs 19 [46.3%], p=0.978. The prevalence of bone marrow edema, periarticular inflammation, and bone erosions was higher in the non-MDA group but did not reach statistical significance: MDA vs non-MDA, n=3 [15.8%] vs 10 [24.4%], p=0.678; n=1 [5.3%] vs 7 [17.1%], p=0.399; n=2 [10.5%] vs 6 [14.6%], p=0.978, respectively. Flexor tenosynovitis was detected only in the non-MDA group (n=10.0, [24%], p=0.047), whereas bone proliferation was detected only in the MDA group (n=3 [15.8%], p=0.048). Comparison of the prevalence of inflammatory MRI findings by grouping the extent of synovitis, bone marrow edema, and periarticular inflammation by severity did not change the results.
Conclusion: This preliminary study results corroborate a high proportion of subclinical inflammation detected by MRI in joints of hand in PsA patients in MDA, whereas overall PsAMRIS scores were low in both MDA and non-MDA groups. These results need to be reproduced in a larger cohort.
References:
- Faustini F. Ann Rheum Dis. 2016;75.
- Coates LC. Ann Rheum Dis. 2010;69.
- Ostergaard M. J Rheumatol 2003;30.
To cite this abstract in AMA style:
Furer V, Polachek A, Mendel L, Levartovsky D, Wollman J, Aloush V, Kaufman I, Sarbagil-Maman H, Borok S, Berman M, Broyde A, Lahat Y, Zureik M, Nevo S, Paran D, Eshed I, Elkayam O. Evidence of Subclinical Joint Inflammation of Hands by Magnetic Resonance Imaging in Patients with Psoriatic Arthritis in Minimal Disease Activity – Interim Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/evidence-of-subclinical-joint-inflammation-of-hands-by-magnetic-resonance-imaging-in-patients-with-psoriatic-arthritis-in-minimal-disease-activity-interim-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evidence-of-subclinical-joint-inflammation-of-hands-by-magnetic-resonance-imaging-in-patients-with-psoriatic-arthritis-in-minimal-disease-activity-interim-analysis/