Session Information
Date: Wednesday, October 24, 2018
Title: 6W019 ACR Abstract: Measures of Healthcare Quality II: QI in SLE, Gout & JIA (2958–2963)
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
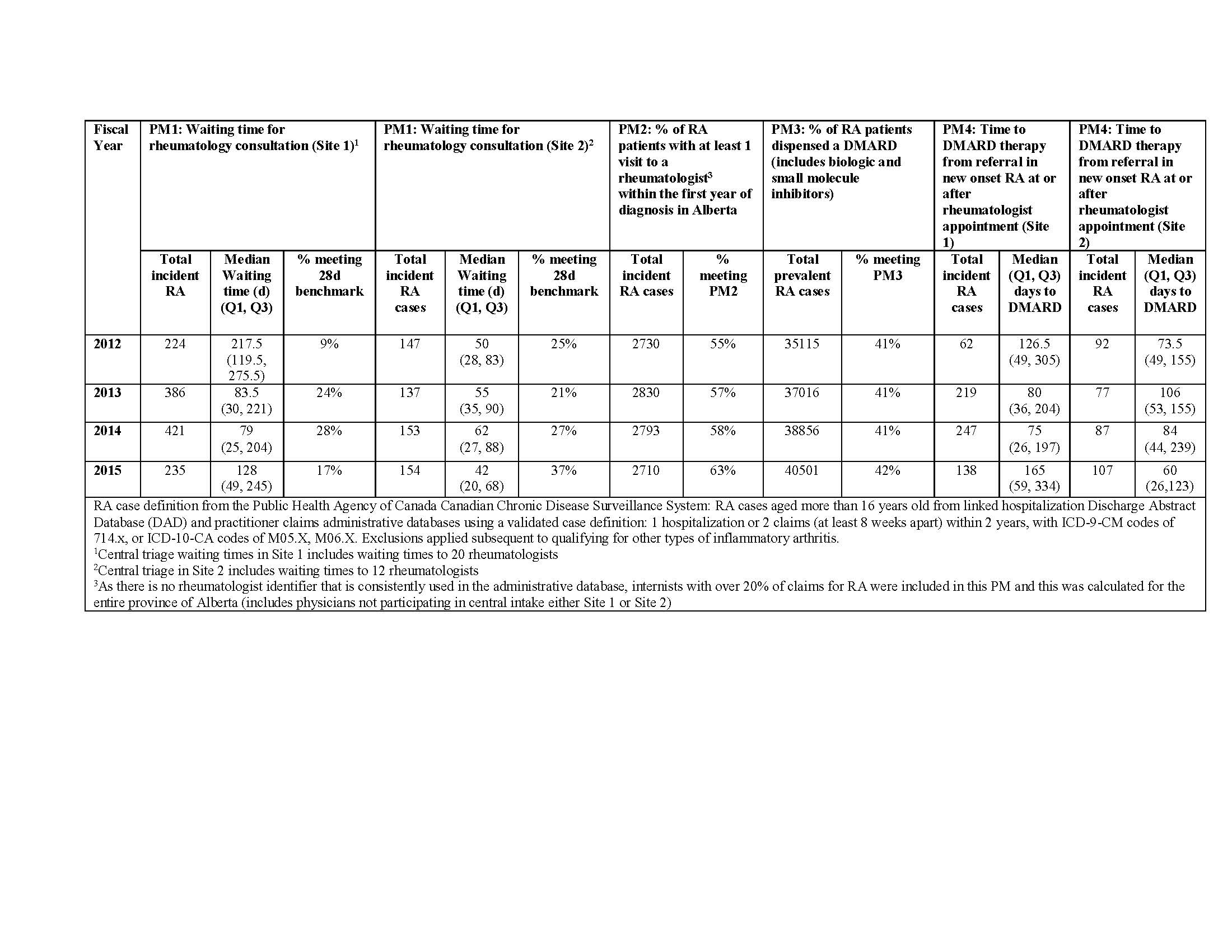
Background/Purpose: Early diagnosis, treatment and ongoing care are critical to optimize RA outcomes. The purpose of the study was to evaluate key elements of RA quality of care using 4 Arthritis Alliance of Canada performance measures (PMs) in Alberta, Canada: PM1) Waiting times for rheumatologist consultation for RA; PM2) Percentage of RA patients with at least one visit to a rheumatologist in the first year of diagnosis; PM3) Percentage of RA patients dispensed a disease modifying anti-rheumatic drug (DMARD); PM4) Time to DMARD initiation.
Methods: All prevalent RA cases 16 years and older between 2002/03 and 2016/17 in AB were defined using 2 or more physician billing codes at least 8 weeks apart and within a 2-year period, or 1 or more hospitalization codes for RA in health administrative data. PMs were estimated through linked datasets for fiscal years 2012-2015. PM1: The wait time in days (d) between referral and first appointment were calculated through linkage with central rheumatology triage databases in two sites. PM2: The percentage of incident RA cases with at least one visit to a rheumatologist within one year of their first RA code. PM3: The percentage of prevalent RA patients dispensed a DMARD (including conventional DMARDs, biologic agents and small molecule inhibitors) was calculated through linkage to a pharmacy database. PM4: Time from RA referral to DMARD dispensation was reported in the calendar year of RA incidence.
Results: The PMs are reported in Table 1 by year and by site where appropriate based on available data sources needed to calculate some measures. Median wait times for rheumatology consultation (PM1) were longer in Site 1 than in Site 2 with between 9-28% meeting the 28-day benchmark in Site 1 and 21-37% in Site 2. Between 2012-2015 the percentage of RA incident cases seen by a rheumatologist within 1 year of onset (PM2) increased from 55 to 63%; however, during this time period the percentage of patients dispensed DMARD therapy (PM3) remained sub-optimal at approximately 40%. Median time to DMARD from referral also suboptimal (PM4).
Conclusion: RA patients in Alberta continue to experience long waiting times to care and treatment with up to 37% of suspected RA cases not seeing a rheumatologist within 1 year of onset. Furthermore, only 40% of RA patients are on DMARD therapy. Further research is warranted to evaluate predictors of adherence to the PMs and to determine the impact on patient outcomes.
To cite this abstract in AMA style:
Barber C, Lacaille D, Faris P, Mosher DP, Katz SJ, Homik J, Patel J, Zhang S, Barnabe C, Hazlewood G, Ahluwalia V, Shiff NJ, Bykerk VP, Twilt M, Benseler S, Burt J, Marshall DA. Evaluation of Performance Measures Reveals Delays and Sub-Optimal Access to Rheumatology Care and Treatment [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-performance-measures-reveals-delays-and-sub-optimal-access-to-rheumatology-care-and-treatment/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-performance-measures-reveals-delays-and-sub-optimal-access-to-rheumatology-care-and-treatment/