Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty has been associated with increased disability and mortality in SLE. To our knowledge, no patient-reported frailty tool has been evaluated alongside a standard frailty measure in SLE. We aimed to assess 1) the prevalence of frailty according to both the standard Fried phenotype (FP) and a validated self-reported frailty instrument, 2) differences between frail and non-frail women according to each definition, 3) the association of each frailty measure with patient-reported disability, and 4) the correlation between frailty definitions.
Methods: Adult women < 70 years old with validated SLE and mild/moderate disease were recruited from a single center. Measures included: frailty (FP and the self-reported FRAIL Scale [FS] [1]); disease activity (SELENA-SLEDAI); disease damage (SLICC/ACR Damage Index); inflammatory/metabolic biomarkers; and patient-reported outcome measures (PROMs), including Valued Life Activities disability. Differences between frail and non-frail participants were evaluated using Fisher’s exact or Wilcoxon rank sum tests and the association of frailty with disability using logistic regression. Correlation between the FP and the FS was determined using Spearman’s correlation.
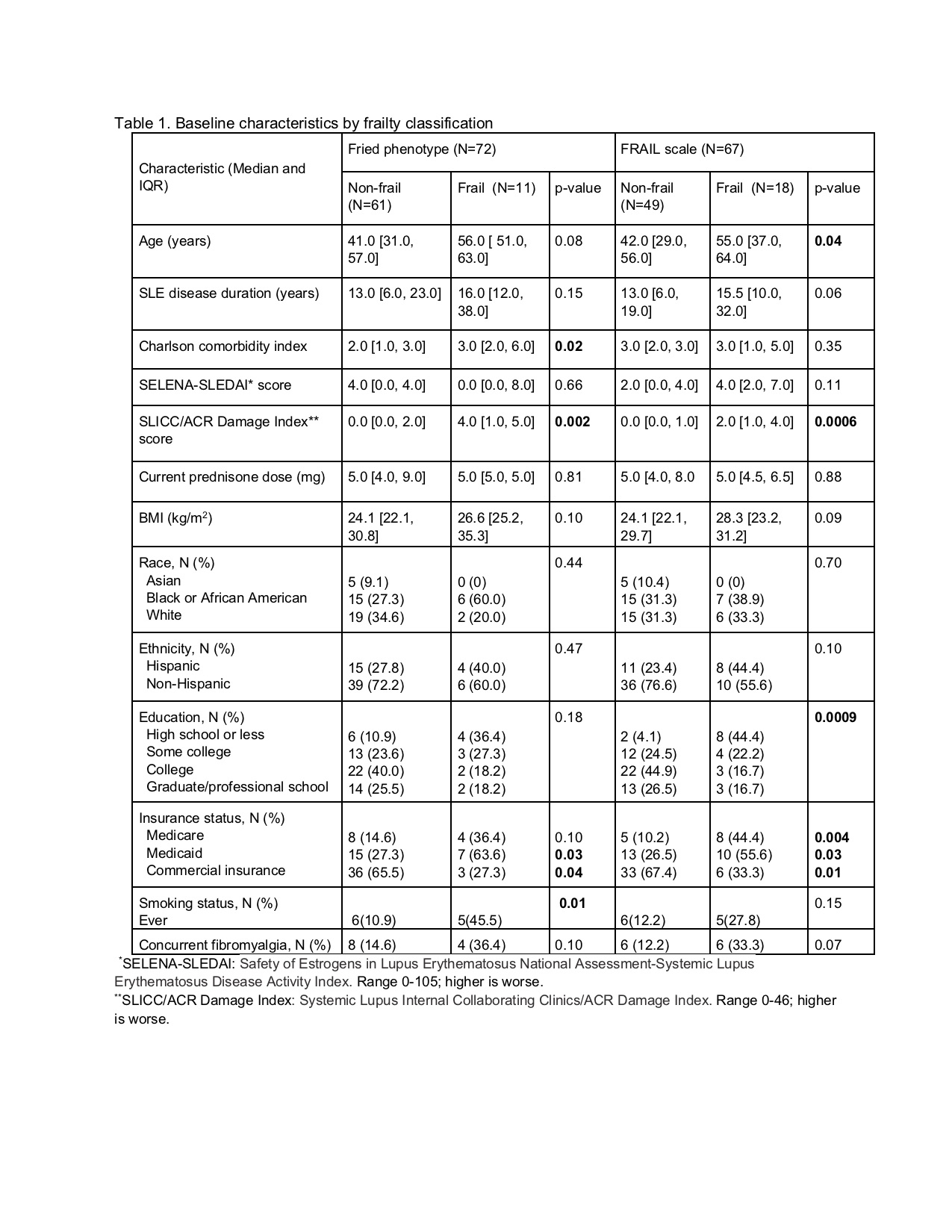
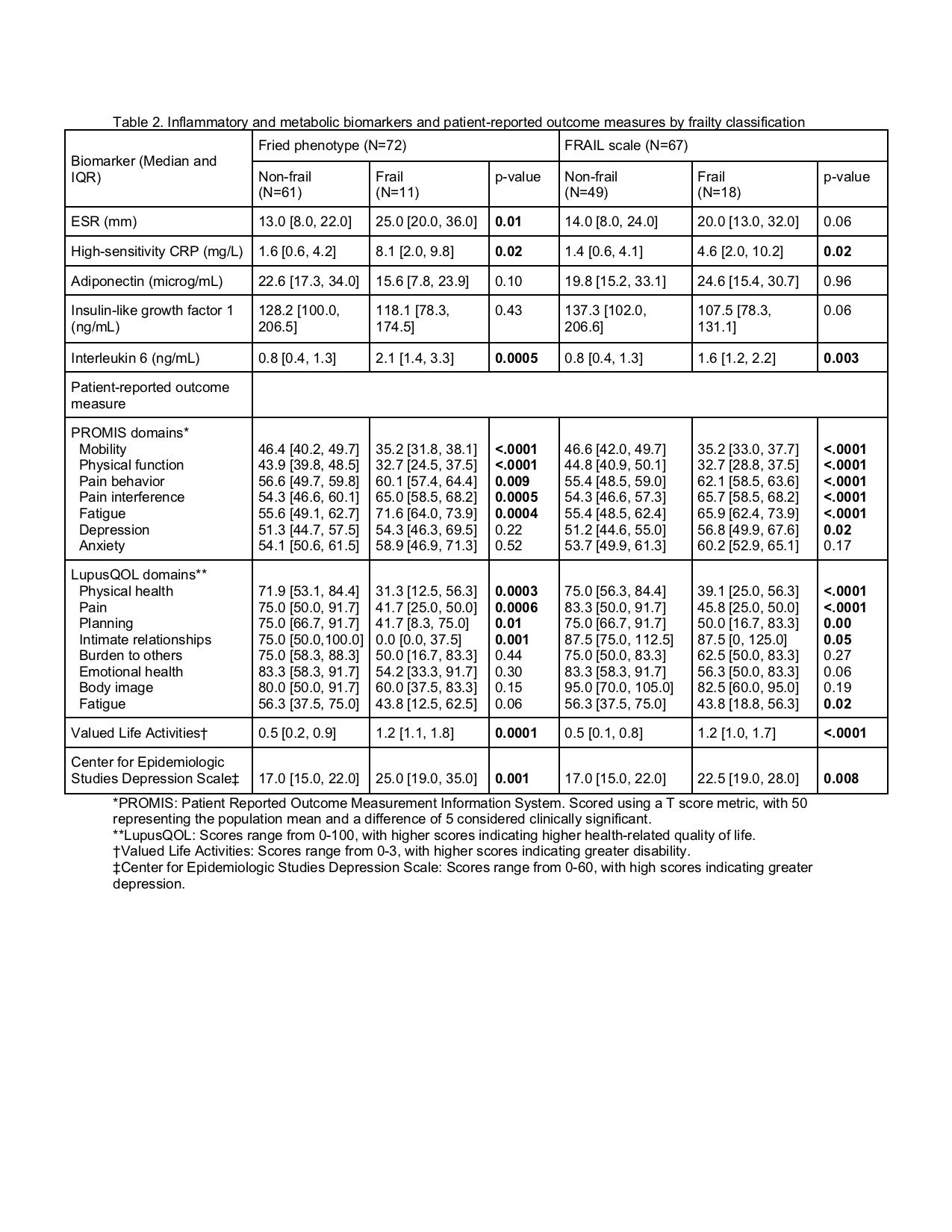
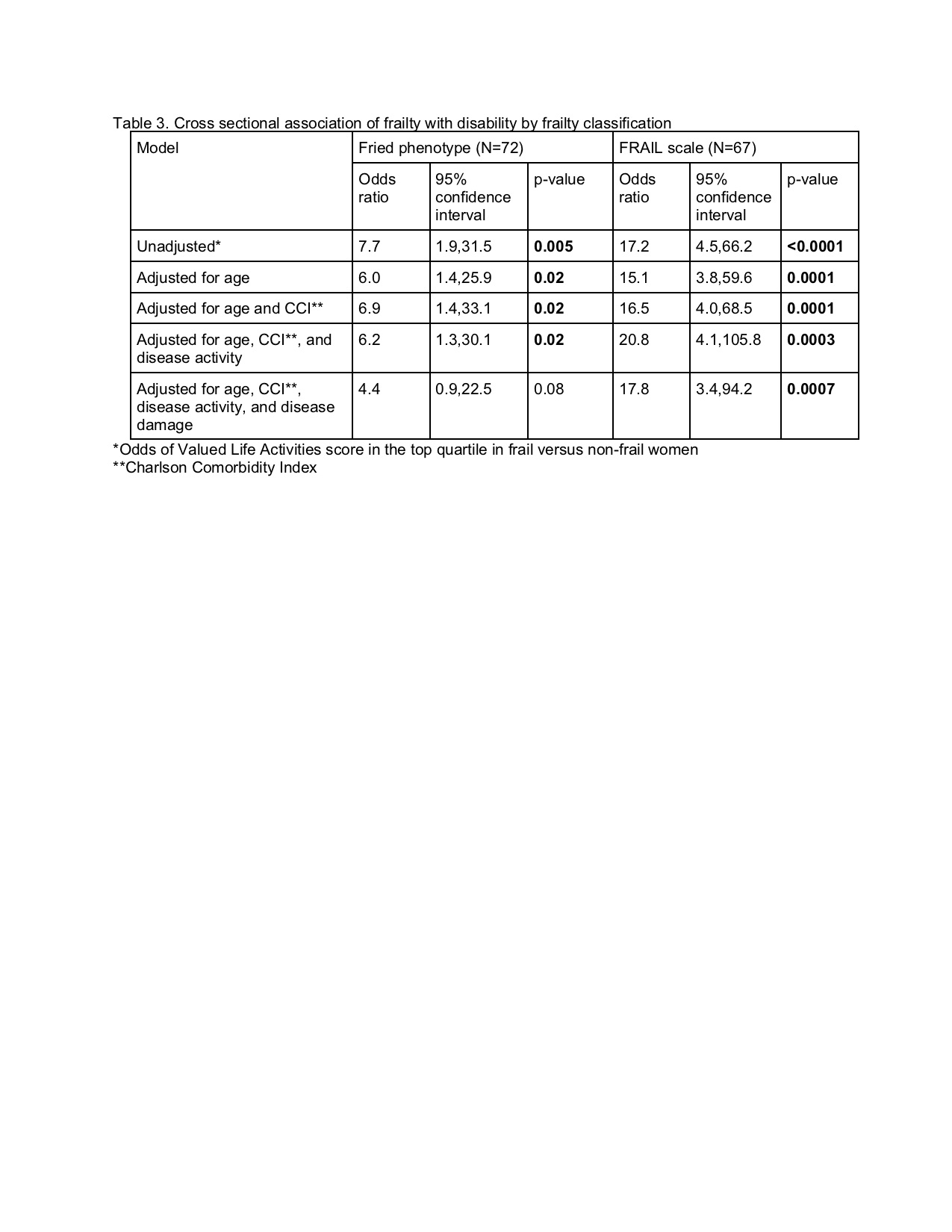
Results: 72 women enrolled; 67 (93%) completed the FS. 17% and 27% were frail according to the FP and the FS, respectively. Frail women according to either definition had greater disease damage (FP: p=0.002; FS: p=0.0006), significantly greater high-sensitivity CRP (FP and FS: p=0.02) and interleukin 6 (FP: p=0.0005; FS: p=0.003), and significantly worse PROMS across multiple domains (Tables 1 and 2). Compared with non-frail women, frail women classified by the FP had greater comorbidity burden (p=0.02), higher prevalence of smoking (p=0.01), and higher ESR (p=0.01); when classified by the FS, frail women were significantly older (p=0.04) with lesser educational attainment (p=0.0009) (Tables 1 and 2). Frailty according to either definition was significantly associated with disability after adjustment for age, comorbidity burden, and disease activity (FP: p=0.02; FS: p=0.0003), but this relationship was attenuated for the FP after adjustment for disease damage (p=0.08) (Table 3). There was moderate correlation between the FS and the FP (r=0.48; p< 0.0001).
Conclusion: The prevalence of patient-reported frailty was high in this cohort of women with SLE. Frail women had generally worse PROMs, providing face validity for both definitions. The FS was strongly associated with disability even after adjustment for multiple confounders. While estimates are imprecise, these data suggest that the FS may be an informative point-of-care tool to identify frail women with SLE.
References:
1. Morley JE et al. J Nutr Health Aging 2012;16:601-8.
To cite this abstract in AMA style:
Lieber S, Paget S, Berman J, Barbhaiya M, Sammaritano L, Kirou K, Carrino J, Nahid M, Rajan M, Sheira D, Mandl L. Evaluation of a Patient-reported Frailty Tool in Women with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/evaluation-of-a-patient-reported-frailty-tool-in-women-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-a-patient-reported-frailty-tool-in-women-with-systemic-lupus-erythematosus/