Session Information
Session Type: Abstract Submissions (ACR)
Reflecting the perceived need for developing evidence-based recommendations on the use of imaging of the joints in the clinical management of spondyloarthritis (SpA) a European League Against Rheumatism (EULAR) task force was convened to develop evidence-based recommendations on the use of imaging of the joints in the clinical management of both axial and peripheral SpA.
Methods:
The task force comprised an expert group of 21 rheumatologists, radiologists and methodologists from 11 countries. Twelve key questions on the role of imaging in SpA were generated using a process of discussion and consensus. Imaging modalities included conventional radiography (CR), ultrasound (US), magnetic resonance imaging (MRI), computed-, positron emission- and single photon emission computed tomography, dual-emission x-ray absorptiometry (DXA) and scintigraphy. Experts used research evidence obtained from a systematic literature review using MEDLINE and EMBASE to develop a set of 10 recommendations. The strength of recommendation (SOR) was assessed by the group members using a visual analogue scale. Quality assessment of the included studies was performed using the QUADAS-2 tool.
Results:
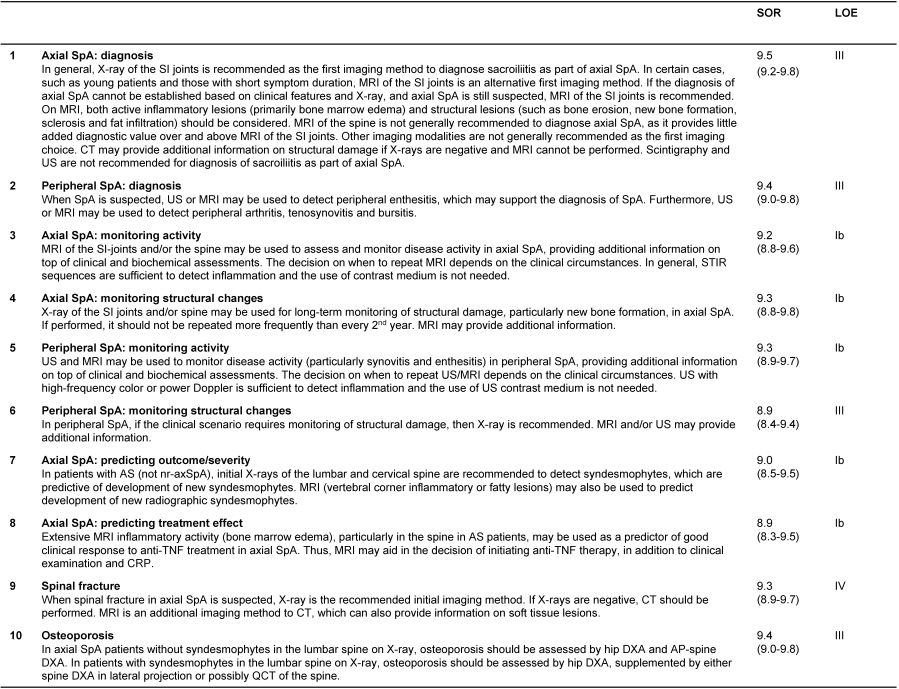
A total of 7550 references were identified in the search process, from which 158 studies were included in the systematic literature review. Ten recommendations were produced encompassing the role of imaging in making a diagnosis of axial- or peripheral SpA, monitoring inflammation and damage, predicting outcome, response to treatment, and detecting spinal fractures and osteoporosis (OP) (Table 1). The SOR for each proposition varied, but was generally very high (mean 8.9-9.5).
Conclusion:
Ten recommendations for the role of imaging in the clinical management of SpA were developed using research-based evidence and expert opinion.
Table 1. EULAR imaging recommendations for spondylarthritis in clinical practice
LOE, level of evidence; categories of evidence: Ia, evidence for meta-analysis of randomized controlled trials; Ib, evidence from at least one randomized controlled trial; IIa, evidence from at least one controlled study without randomization; IIb, evidence from at least one other type of quasi-experimental study; III, evidence from non-experimental descriptive studies, such as comparative studies, correlation studies and case–control studies; IV, evidence from expert committee reports or opinions or clinical experience of respected authorities, or both. CRP, C-reactive protein; CT, computed tomography; DXA, dual-energy X-ray absorptiometry; MRI, magnetic resonance imaging; nr-axSpA, non-radiographic axial spondyloarthritis; SI, sacroiliac; SpA, spondyloarthritis; SOR, strength of recommendation, mean (range) of visual analogue scale; STIR, short tau inversion recovery; TNF, tumor necrosis factor alpha; US, ultrasonography;
Disclosure:
P. Mandl,
None;
V. Navarro-Compán,
None;
P. Bakker,
None;
L. Terslev,
None;
P. Aegerter,
None;
D. van der Heijde,
None;
M. A. d’Agostino,
None;
X. Baraliakos,
MSD, Pfizer, Abbvie,
2,
Abbott/Abbvie, Centocor, Janssen, Merck, Pfizer, Schering-Plough, Roche UCB, and Wyeth,
5;
S. J. Pedersen,
None;
A. G. Jurik,
None;
E. Naredo,
MSD, Spanish Foundation of Rheumatology,
8,
Abbvie, Roche Pharma, BMS, Pfizer, UCB, GE, ESAOTE,
8;
C. Schueller-Weidekamm,
None;
U. Weber,
Abbott Laboratories,
5;
M. Wick,
None;
E. Filippucci,
None;
P. G. Conaghan,
Abbvie, Janssen, Novartis, Pfizer, Roche,
5,
Abbvie, Merck, Pfizer, Roche, UCB,
8;
M. Rudwaleit,
Roche, MSD, Pfizer, Novartis, UCB,
5,
AbbVIe, BMS, Chugai,
8;
G. A. Schett,
None;
J. Sieper,
None;
S. Tarp,
None;
H. Marzo-Ortega,
AbbVie, MSD, Janssen, Pfizer, UCB,
8;
M. Ostergaard,
Abbott/Abbvie, Centocor, Merck, Schering-Plough,
2,
Abbott/Abbvie, BMS, Boehringer-Ingelheim, Eli-Lilly, Centocor, GSK, Janssen, Merck, Mundipharma, Novo, Pfizer, Schering-Plough, Roche UCB, and Wyeth,
5.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/eular-recommendations-for-the-use-of-imaging-in-spondyloarthritis-in-clinical-practice/