Session Information
Date: Tuesday, November 10, 2015
Title: Spondylarthropathies and Psoriatic Arthritis - Clinical Aspects and Treatment Poster III: Therapy
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The role of co-medication e.g. with conventional synthetic disease-modifying
antirheumatic drugs (csDMARDs), among patients with psoriatic arthritis (PsA)
who are receiving tumor necrosis factor inhibitors (TNFi) remains unclear. Some
studies have indicated a beneficial role in the longevity of treatment,
potentially by reducing the formation of anti-drug antibodies. Etanercept has
generally been found to be less immunogenic than monoclonal antibody TNFi. This
study aimed to investigate the role of concomitant methotrexate on drug
survival of etanercept in psoriatic arthritis (PsA).
Methods: We
included consecutive PsA patients from a Norwegian out-patient clinic. Baseline
characteristics and drug survival were compared between patients with and
without methotrexate co-medication. The X2 test, independent
t-test and Mann-Whitney U test were applied as appropriate for group
comparisons. Drug survival was explored by Kaplan-Meier analysis, and patients
receiving and not receiving co-medication were compared using the log rank
test. Cox regression analysis was used to identify predictors of
discontinuation.
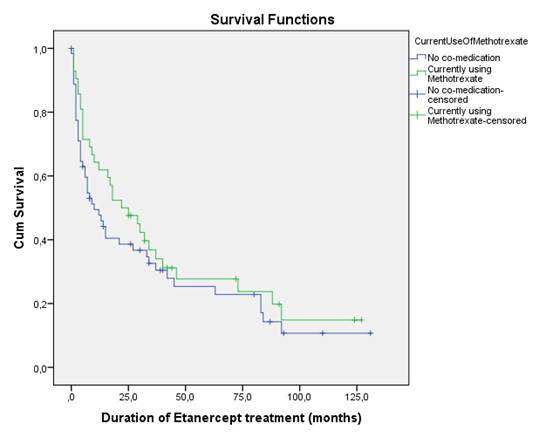
Results: We included 105 patients
treated with etanercept, 42 receiving co-medication with methotrexate. Mean
(SD) age was 54,3 (11,0) years, years of education 13,1 (3,7), disease duration
13,4 (8,8) years, body mass index 28,2 (4,8) kg/m2, baseline CRP 11,1
(23,4), baseline swollen joints 2,9 (3,4), 42,9% were female and 21,9% currently
smoking. Overall, 31 (29,5%) patients were previously treated with TNFi. Baseline
characteristics were similar for patients with and without co-medication. Drug
survival of etanercept was similar for patients receiving versus not receiving concomitant
methotrexate (log rank test p=0,277, figure). In the Cox regression analysis
the only identified predictor for etanercept discontinuation was previous use
of TNFi. Separate analyses for first time TNFi users did not change the primary
outcome.
Conclusion: In our population of etanercept treated PsA patients, we found
similar drug survival for patients with and without co-medication with methotrexate.
The only identified predictor for etanercept discontinuation was previous use
of TNFi.
To cite this abstract in AMA style:
Michelsen B, Soldal DM, Kavanaugh A, Haugeberg G. Etanercept Treatment in Psoriatic Arthritis: Need for Co-Medication? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/etanercept-treatment-in-psoriatic-arthritis-need-for-co-medication/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/etanercept-treatment-in-psoriatic-arthritis-need-for-co-medication/