Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is a connective tissue disease with pulmonary involvement seen in 75% of patients and esophageal involvement in 90% of the patients. Pulmonary disease has overtaken renal disease as the leading cause of death. There is conflicting evidence about the association between esophageal dysmotility and lung involvement. We aimed to evaluate the relationship between esophageal dysmotility and lung disease by correlating the results of Esophageal transit time (ETT) with pulmonary function test (PFT).
Methods: Charts of SSc patients fulfilling 2013 ACR/EULAR classification criteria seen in Rheumatology from 2004 to 2015 were reviewed. Patients demographics, laboratory, results of ETT, High resolution CT (HRCT) of lung and PFT were collected at baseline, years 1, 3, 5 and 10. Patients were divided based on their initial ETT findings. Using the linear mixed effects model, we tested the effect of ETT status on forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCo) and estimated the progression rates in two groups. We adjusted for relevant covariates such as disease sub type, smoking, obesity and medications.
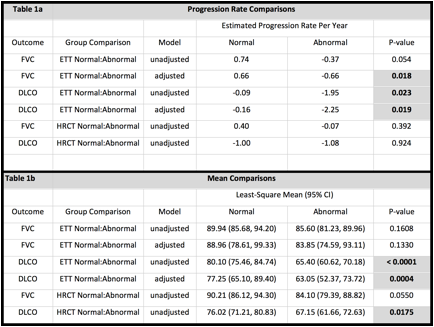
Results: 130 patients were identified with either LcSSC (109) or diffuse SSc (21). ETT was normal in 67(52%) and abnormal in 63(48%) patients. At baseline, years 1,3,5 and 10, the mean DLCo was significantly different between the groups while the mean FVC was not. An error bar graph indicating mean and standard error of mean at each year is provided for each outcome. Abnormal ETT group have a significantly worse progression of DLCo, both in unadjusted (p=0.023) and adjusted (p=0.019) models but FVC progression was significantly worse in adjusted (p=0.018) model only. The estimated progression rates per year are provided in Table 1a. The effect of ETT status on FVC is statistically insignificant for both unadjusted (p= 0.1608 and adjusted (p= 0.133) but significant for DLCo (unadjusted p= 0.0004, adjusted p=0.0175). The means and 95% confidence intervals for the two groups are provided in Table 1b. Patients with baseline abnormal HRCT had significantly lower DLCo but did not have worse progression rate.
Conclusion: Our results show that presence of abnormal ETT correlates with reduced mean DLCo and worsening of FVC and DLCo over a period of 10 years. Presence of abnormal HRCT at baseline did not indicate progression of FVC or DLCo. Larger prospective studies need to be done to find a causal relationship. References: 1. Steen VD et al: Ann Rheum Dis 66, 2007.
2. Christmann RB et al: Semin Arthritis Rheum. 2010 Dec; 40(3). 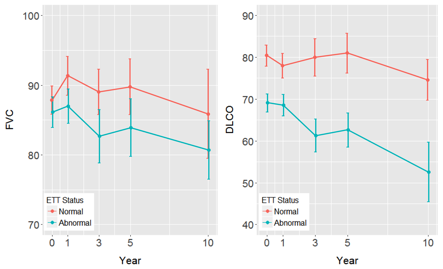
To cite this abstract in AMA style:
Kishore S, Lakshminarayanan S, Kuo CL, Mandhadi R. Esophageal Dysmotility and Interstitial Lung Disease in Patients with Scleroderma: A Retrospective Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/esophageal-dysmotility-and-interstitial-lung-disease-in-patients-with-scleroderma-a-retrospective-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/esophageal-dysmotility-and-interstitial-lung-disease-in-patients-with-scleroderma-a-retrospective-study/