Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Orthopaedic
shoes (OS) may help to reduce pain and increase activity participation in
rheumatoid arthritis (RA) patients, but should ideally not be needed. We investigated
the prevalence and potential risk factors of OS use in RA patients after 10
years of targeted treatment.
Methods: In the 4 treatment arms of the BeSt study, 508 patients with
recent onset RA were treated aiming at disease activity score (DAS) ≤2.4. After 10 years, patients were
asked if they used OS. Baseline characteristics of users and non-users were
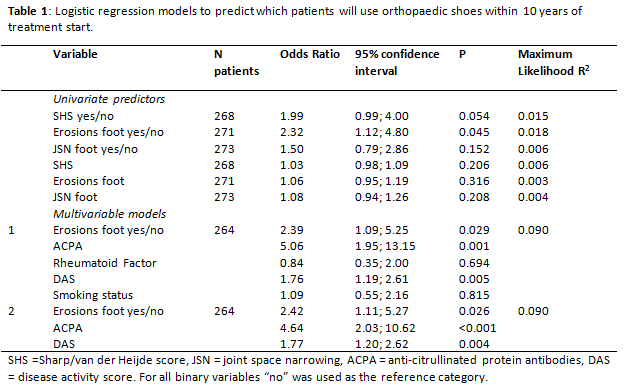
compared. Univariable binary logistic regression was performed with OS use as
outcome, and baseline total Sharp/van der Heijde score (SHS), foot erosions and
foot joint space narrowing (JSN) as continuous and dichotomous variables (cut-off
≥1) as potential predictors. Next, statistically significant predictors
(p<0.1) were tested in a multivariable model simultaneously with rheumatoid
factor (RF), smoking status, anti-citrullinated protein antibodies (ACPA) and DAS. Timing of OS use being unavailable,
non-baseline factors were not considered. For highly correlated variables both
associated with OS use, only the strongest contributing variable was added to
the model. Predictors with statistically significant contribution
were kept in the final model. Interaction of each predictor with treatment arm
was tested and ruled out.
Results: Of 285/508 patients (56%) information was available regarding OS
use at year 10. Responders to the question were younger than non-responders [age
mean (SD) 51.3 (12.0) vs 58.4 (14.8) years, p<0.001], but were similar regarding
gender, smoking status, ACPA, DAS, SHS, JSN and erosions (all baseline). Twenty-one
percent (57/273) of the patients reported OS use after 10 years [68.4% female,
mean (SD) age 50.3 (11.0) years, DAS 4.6 (0.9), SHS 4.7 (5.3), erosions 1.0
(2.3), JSN 1.0 (1.9), ACPA+ 83.3%, RF+ 77.2%, all baseline]. OS users were more
often ACPA+ (77.2% vs 65.8%) and had more erosions [mean (SD) 1.25 (2.4) vs 0.48
(2.5), all p<0.05]. Univariable logistic regression showed that only foot erosions
contributed significantly to the model as binary (OR 1.95, CI95: 1.1-4.8) but
not as continuous variable (OR 1.06, CI95: 0.9-1.2). Neither total SHS nor foot-JSN
(binary or continuous) contributed significantly to the model. Multivariable
logistic regression showed that baseline foot erosions (binary; OR 1.85, CI95: 1.1-5.3),
ACPA+ (OR 4.88, CI95: 2.0-10.6) and DAS (OR 1.72, CI95: 1.2-2.6) were
independent predictors of OS use after 10 years. Combining baseline foot
erosions, ACPA+ and baseline DAS created the best model.
Conclusion: Despite 10 years of DAS≤2.4 targeted treatment, 21% of
recent onset RA patients with available data after 10 years used OS. Presence
of foot erosions at treatment start predicts OS use after 10 years; the risk increases
for ACPA+ patients and to a lesser extent for patients with higher baseline DAS.
To cite this abstract in AMA style:
Bergstra SA, van den Berg R, Riyazi N, Steup-Beekman GM, van der Lubbe PAHM, Kerstens PJSM, Lems WF, Huizinga TWJ, Landewé RBM, Allaart CF. Erosions in the Foot at Baseline Are Predictive of Orthopedic Shoe Use after 10 Years of Treat to Target Therapy [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/erosions-in-the-foot-at-baseline-are-predictive-of-orthopedic-shoe-use-after-10-years-of-treat-to-target-therapy/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/erosions-in-the-foot-at-baseline-are-predictive-of-orthopedic-shoe-use-after-10-years-of-treat-to-target-therapy/