Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: As of May 2021, Canada had reached over 1.3 million confirmed cases of SARS-CoV-2 infection, and over 25,000 deaths. This study identified children in Canada hospitalized with paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 infection (PIMS), also known as multisystem inflammatory syndrome in children (MIS-C), and aimed to 1) Describe clinical and laboratory features at presentation, management, outcomes, and 2) Identify risk factors for intensive care unit (ICU) admission.
Methods: We conducted a national prospective study using the infrastructure of the Canadian Paediatric Surveillance Program (CPSP), a network of >2,800 paediatricians across Canada. Physicians reported cases of hospitalized children who met study criteria from March 2020-May 2021, through a weekly online questionnaire distributed via the CPSP network. Cases were categorized as confirmed MIS-C, presumed MIS-C, and/or confirmed PIMS defined in Figure 1. Modified Poisson regression analysis was used to compute adjusted risk ratios (aRR) for ICU risk factors associated with PIMS/MIS-C.
Results: A total of 506 cases of children hospitalized with PIMS/MIS-C were reported during the study period, of which 383 unique cases were included in the primary analysis (161 confirmed MIS-C, 202 presumed MIS-C, and/or 352 confirmed PIMS) with the majority of cases being reported from the provinces of Ontario (44.6%) and Quebec (39.7%). A total of 167/383 (43%) cases had a SARS-CoV-2 link (62.3% close contact, 58.1% positive PCR, 32.3% known positive serology). Of the 216 cases (56%) with no known link, 55/114 with serology results available were negative. Majority were preschool (1-5 years) or school aged (6-12 years), with slight male predominance (57.7%), and were previous healthy (60 (15.7%) with co-morbidities). Median duration of fever was 6 days; 283/383 (74%) had gastrointestinal involvement; more than half had mucocutaneous changes including rash (64.5%), bilateral non-exudative conjunctivitis (62.9%), and changes in lips/oral cavity (58.7%). Laboratory features indicated hyperinflammation (Table 1).
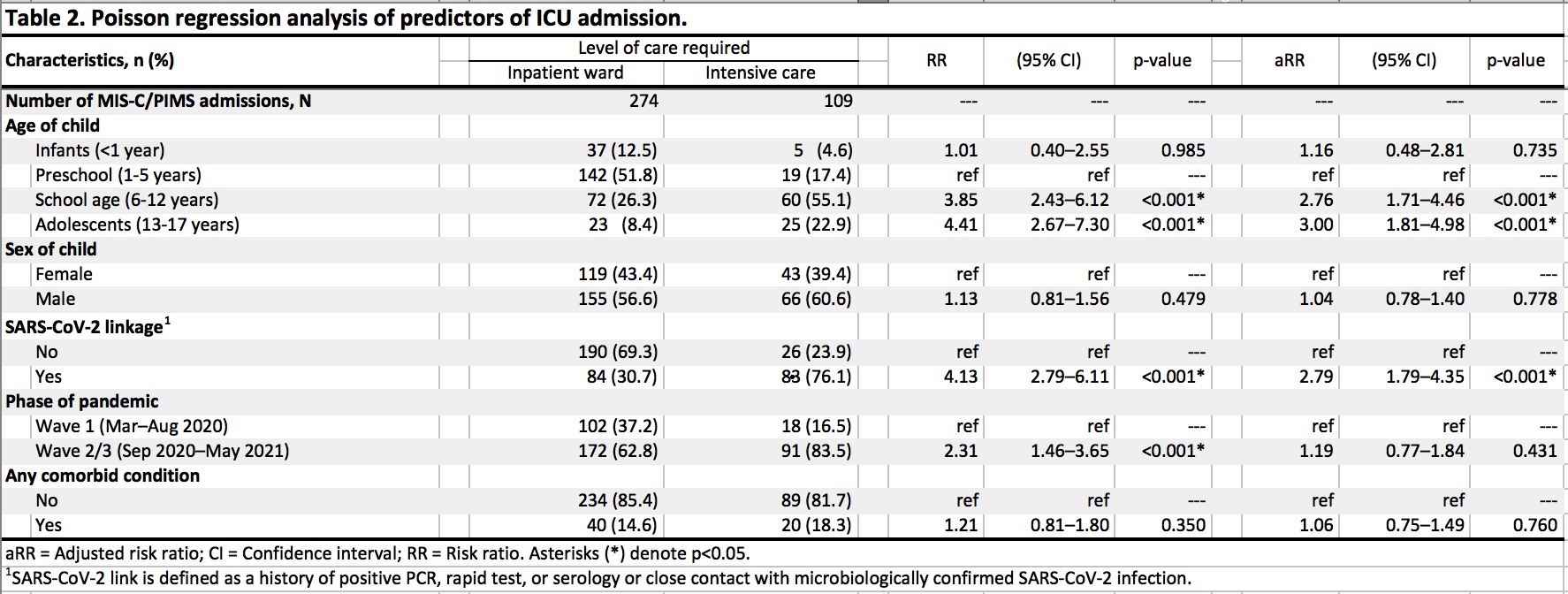
Shock/hypotension was reported in 125 (32.6%). There were no deaths. Cardiac involvement with abnormal echocardiograms was reported in 161/366 (44%) including decreased heart function (14.5%), coronary dilatation (9.1%) and aneurysms (13.1%). Almost one third (28.5%) required ICU admission, with 25.1% requiring respiratory/hemodynamic support. For treatment, 235 (61%) received both IVIG and corticosteroids, 111 (29%) received IVIG only, 7 (1.8%) received corticosteroids only, 30 (7.8%) received neither, and 18 (4.7%) received biologics. Risk factors for ICU admission included presence of SARS-CoV-2 link (aRR 2.79, 95% CI 1.79-4.35; p < 0.001) and older age groups: school aged (aRR 2.76, 95% CI 1.71-4.46; p < 0.001) and adolescents (13-17 years) (aRR 3.00, 95% CI 1.81-4.98; p < 0.001); while no association found with sex or comorbidity (Table 2).
Conclusion: This national prospective study reports on the largest series of children hospitalized with PIMS/MIS-C in Canada, providing insight on overall severity and at–risk groups that is essential for prompt recognition and management.
 Figure 1. Flow chart of participants meeting the case definitions for MIS-C and PIMS. Confirmed MIS-C: meets MIS-C criteria (adapted by the World Health Organization (WHO))a AND no other cause identified AND SARS-COV_2 link present (defined as a history of positive PCR, rapid test, or serology or close contact with microbiologically confirmed SARS-CoV_2 infection); Presumed MIS-C: same as confirmed MIS-C except no known SARS-CoV_2 link; Confirmed PIMS: meets study criteria (1) fever ≥3 days (2) elevated inflammatory markers (C-reactive protein (CRP) ≥ 30 mg/L, Erythrocyte sedimentation rate (ESR) ≥ 40 mm/h OR Ferritin ≥ 500 μg/L) (3) one or both: features of Kawasaki disease or toxic shock syndrome AND (4) no other cause identified. a https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid_19 1Of confirmed PIMS cases, 150 also met criteria for confirmed MIS-C, 182 also met criteria for presumed MIS-C, while 20 did not meet criteria for MIS-C. Six cases met criteria for confirmed or presumed MIS-C but not confirmed PIMS.
Figure 1. Flow chart of participants meeting the case definitions for MIS-C and PIMS. Confirmed MIS-C: meets MIS-C criteria (adapted by the World Health Organization (WHO))a AND no other cause identified AND SARS-COV_2 link present (defined as a history of positive PCR, rapid test, or serology or close contact with microbiologically confirmed SARS-CoV_2 infection); Presumed MIS-C: same as confirmed MIS-C except no known SARS-CoV_2 link; Confirmed PIMS: meets study criteria (1) fever ≥3 days (2) elevated inflammatory markers (C-reactive protein (CRP) ≥ 30 mg/L, Erythrocyte sedimentation rate (ESR) ≥ 40 mm/h OR Ferritin ≥ 500 μg/L) (3) one or both: features of Kawasaki disease or toxic shock syndrome AND (4) no other cause identified. a https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid_19 1Of confirmed PIMS cases, 150 also met criteria for confirmed MIS-C, 182 also met criteria for presumed MIS-C, while 20 did not meet criteria for MIS-C. Six cases met criteria for confirmed or presumed MIS-C but not confirmed PIMS.
To cite this abstract in AMA style:
El Tal T, Morin M, Morris S, Berard R, Farrar D, Kakkar F, Moore-Hepburn C, Haddad E, Scuccimarri R, Yeung R. Epidemiology and Disease Burden of Hospitalized Children with Paediatric Multisystem Inflammatory Syndrome Temporally Associated with SARS-CoV-2 Infection in Canada: A Canadian Pediatric Surveillance Program National Prospective Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/epidemiology-and-disease-burden-of-hospitalized-children-with-paediatric-multisystem-inflammatory-syndrome-temporally-associated-with-sars-cov-2-infection-in-canada-a-canadian-pediatric-surveillance/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-disease-burden-of-hospitalized-children-with-paediatric-multisystem-inflammatory-syndrome-temporally-associated-with-sars-cov-2-infection-in-canada-a-canadian-pediatric-surveillance/