Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
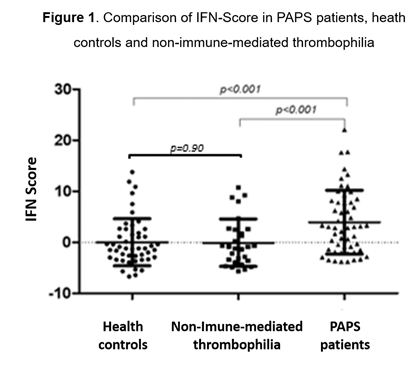
Background/Purpose: Primary antiphospholipid syndrome (PAPS) is an autoimmune vasculopathy mediated by autoantibodies with thrombosis as its main clinical manifestation. The presence of antiphospholipid antibodies, while relevant to confirm the diagnosis, does not seem to be sufficient to fully explain the pathophysiology and a second trigger is usually needed. Besides the hypotheses of viral infections and inflammatory insult as possible triggers, type I Interferon (IFN) has been pointed as a possible protagonist. Recently, two studies have demonstrated that a relevant percentage of PAPS patients have an up-regulation of IFN genes in peripheral blood mononuclear cells (PBMC). However, 20% and 28% of patients in these 2 cohorts, had anti-dsDNA positive antibodies, a highly specific Systemic Lupus Erythematosus (SLE) autoantibody. The aim of this study is to determine the prevalence of type I IFN signature in PBMC of patients with PAPS without specific SLE autoantibodies and search for it with clinical and laboratorial associations. Methods: 53 PAPS patients (according to Sydney´s criteria) were consecutively selected and age-matched with 50 healthy controls. A third group, with non-immune-mediated thrombophilia patients, was also included. The expression of 41 IFN induced genes was analysed using real time quantitative PCR (TaqMan Low Density Array). A principal component analysis (PCA) was used to determine which genes should compose the IFN signature and z-score was calculated. The IFN signature score cut-off was defined with a ROC curve, as the point that maximized both the specificity and sensitivity. Clinical and laboratorial features were analysed searching for associations with IFN signature. Results: 11 IFN genes were highly expressed in primary APS patients. After PCA, 6 genes remained in the IFN signature: DNAJA1, IFIT5, IFI27, MX1, IFI6, TYK2. The type I IFN signature was present in 49% of patients with primary APS compared to 14.0% of healthy controls and 17% of non-immune-mediated thrombophilia patients (p<0,0001). The mean IFN score was significantly higher in PAPS patients (4.0 fold higher, p<0.0001) than in controls (Figure 1). A higher IFN signature was associated with a younger age at the first APS event (p=0.023) and with the presence of obstetric events, especially with preeclampsia (p=0.032). Treatment with statins was associated with lower levels of IFN scores (p=0.026). Conclusion: Our result indicates that PAPS patients, without lupus specific antibodies, have an enhanced type I IFN gene signature, not observed in non-immune mediated thrombophilia. We also provide novel data demonstrating that this overexpression of type I IFN-regulated genes is associated with an earlier onset of APS events and preeclampsia. Further studies are necessary to determine if this subgroup of patients will benefit of interventions targeting the type I IFN signalling pathway.
To cite this abstract in AMA style:
Lopes M, Torrezan G, Gandara AP, Olivieri E, Nascimento I, Okazaki E, Bonfa E, Carraro D, Andrade D. Enhanced Type I Interferon Gene Signature in Primary Antiphospholipid Syndrome: Association with Earlier Disease Onset and Preeclampsia [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/enhanced-type-i-interferon-gene-signature-in-primary-antiphospholipid-syndrome-association-with-earlier-disease-onset-and-preeclampsia/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/enhanced-type-i-interferon-gene-signature-in-primary-antiphospholipid-syndrome-association-with-earlier-disease-onset-and-preeclampsia/
