Session Information
Session Type: Abstract Submissions (ACR)
Elevated serum anti-flagellin antibodies implicate subclinical bowel inflammation in ankylosing spondylitis
Background/Purpose:
Ankylosing spondylitis (AS) and inflammatory bowel disease (IBD) share genetic and clinical features. IBD is associated with the presence of antibodies to a variety of commensal microorganisms including anti-Sacchoaromyces cerevesiae antibodies (ASCA), antineutrophil cytoplasmic antibodies (ANCA), anti-I2 (associated with anti-Pseudomonas activity), anti-E. coli outer membrane porin C (anti-OmpC) and anti-flagellin antibodies (anti-CBir1). Subclinical intestinal inflammation may be present in up to 65% of patients with AS. This study evaluated the presence of antimicrobial antibodies in patients with AS alone, patients with AS and concomitant IBD (AS-IBD) and a control group of patients with mechanical back pain (MBP).
Methods:
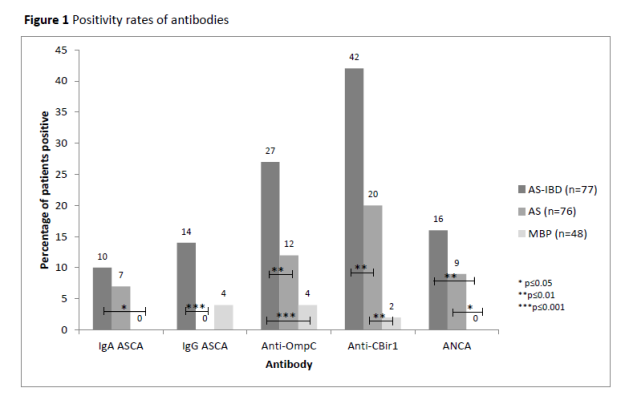
Patients with AS-IBD were identified from a longitudinal prospective AS cohort and matched by age and disease duration to patients with AS alone. Sera were tested by ELISA for ASCA IgG and IgA, anti-OmpC, anti-CBir1 and ANCA in 76 patients with AS alone, 77 patients with AS-IBD and 48 patients with MBP (who underwent clinical, laboratory and radiological investigation to exclude spondyloarthritis). Antibody positivity rates, median quantitative antibody levels and the proportion of patients with antibody levels in the 4th quartile of a normal distribution were compared between the three groups of patients.
Results:
Antibody positivity rates are shown in Figure 1. Patients with AS alone demonstrated higher anti-CBir1 antibody positivity rates (19.7% versus 2.1%, p=0.005) and median antibody levels (15.0 [10.0-23.8] EU versus 10.0 [7.0-15.0] EU, p=0.0007) than MBP patients. AS-IBD patients demonstrated elevated responses when compared to AS alone for ASCA, anti-OmpC and anti-CBir1. Quartile analysis confirmed the findings. Acute phase reactants were significantly elevated in anti-CBir1 positive patients compared to anti-CBir1 negative patients: median (IQR) CRP 11.5 (5.3-20.5)mg/L versus 6.0 (3.0-15.5)mg/L (p=0.006); median (IQR) ESR 19.0 (8.5-32.0)mm/h versus 8.0 (3.0-18.0)mm/h (p<0.001). Among patients with AS alone, acute phase reactants remained significantly elevated in anti-CBir1 positive patients compared to anti-CBir1 negative patients (median (IQR) CRP 14.0 (7.0-19.0)mg/L versus 3.0 (3.0-15.0)mg/L, p=0.033); median ESR (IQR) 26.0 (10.0-33.0)mm/h versus 5.0 (3.0-20.0)mm/h). No significant difference was seen in acute phase reactants between anti-CBir 1 positive and negative patients within the AS-IBD group.
Conclusion:
These data suggest that adaptive immune responses to microbial antigens occur in AS patients without clinical IBD and support the theory of mucosal dysregulation as a mechanism underlying the pathophysiology of AS.
Disclosure:
D. Wallis,
None;
A. Asaduzzaman,
None;
M. H. Weisman,
None;
N. Haroon,
None;
A. Anton,
None;
D. P. B. McGovern,
None;
S. R. Targan,
None;
R. D. Inman,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/elevated-serum-anti-flagellin-antibodies-implicate-subclinical-bowel-inflammation-in-ankylosing-spondylitis/