Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Electrocardiographic Abnormalities Are Associated with the Occurrence of Strokes in Systemic Lupus Erythematosus
Background/Purpose: Systemic lupus erythematosus (SLE) patients have a 10-fold higher risk for myocardial infarctions and a 3-fold higher risk for congestive heart failure and strokes, making cardiovascular disease (CVD) the leading cause of death in SLE. In the general population, nonspecific ST-T and QTc abnormalities are strong predictors of CV mortality. Yet, studies exploring the value of the ECG in identifying SLE patients at increased risk for cardiovascular events (CVE) are lacking. Therefore, we investigated the association between electrocardiographic (ECG) abnormalities and CVE in SLE.
Methods: We retrospectively reviewed 12-lead ECG data preceding a diagnosis of cardiovascular event (defined as myocardial infarction, congestive heart failure, and/or stroke) in 81 SLE patients, compared with ECG data from 269 SLE patients lacking a diagnosis of CVE. Patients were identified by ICD-9 & 10 codes for SLE, and the diagnosis was ascertained by chart review confirming ≥ 4 revised 1997 ACR or SLICC classification criteria. CVE were similarly confirmed by chart review including cardiology notes, diagnostic tests, and procedure data confirming the events. Nonspecific ST-T abnormalities were defined by the Minnesota code, and the QT interval was calculated and adjusted for heart rate by Bazett’s formula. Regression models were constructed to test the association of ECG abnormalities with CVE.
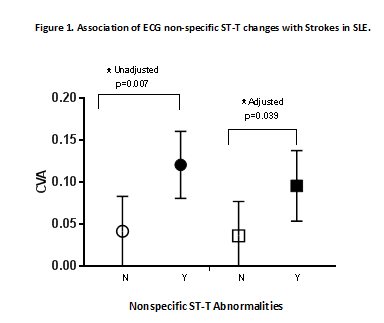
Results: The mean age was 47±15 years, 90% were female, 43% Hispanic and 40% were black. Sixty-five percent had hypertension, 8% had diabetes, 16% had a history of smoking, and 17% had hyperlipidemia. Mean disease duration at the time of the CVE was 12 (±10) years. Nonspecific ST-T abnormalities were seen in 65% and 48% of patients with and without CVE, respectively (OR=2.05, p= 0.006). Mean QTc length was 435 and 431 ms in those with and without CVE, respectively (p=0.0102); and the maximum QTc length was 464 and 431 ms, respectively (p=0.0207). After adjusting for confounders, the association between any CVE and ECG abnormalities lost significance. However, strokes remained significantly associated with nonspecific ST-T changes (OR=2.45, 95% CI:1.01, 5.98; p=0.05) and a maximum QTc≥440 ms (OR= 3.05, 95% CI: 1.02, 9.10; p= 0.045) after adjusting for hypertension (Figures 1 & 2).
Conclusion: ECG nonspecific ST-T abnormalities and a maximum QTc≥440 ms were associated with a 2-3-fold higher risk for strokes in SLE patients. This study supports the use of ECG to identify SLE patients at risk for stroke.
To cite this abstract in AMA style:
Perez T, Depender C, Li J, Geraldino-Pardilla L. Electrocardiographic Abnormalities Are Associated with the Occurrence of Strokes in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/electrocardiographic-abnormalities-are-associated-with-the-occurrence-of-strokes-in-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/electrocardiographic-abnormalities-are-associated-with-the-occurrence-of-strokes-in-systemic-lupus-erythematosus/