Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: As patients with rheumatic diseases (RDs) growing into a large population globally, concerns continue exist regarding the potential development of tuberculosis (TB) in this group, since proximately 1/4 to 1/3 people have latent tuberculosis infection (LTBI) and the risk of developing active tuberculosis (ATB) in immunocompromised patients are 2 to 10 times higher. World Health Organization have recommended TB preventive treatment (TPT) in patients at high-risk but the effectiveness has never been systematically summarized. We here assessed systematically the effectiveness of TPT in patients with RDs.
Methods: A systematic literature search was conducted in PubMed, Embase, the Cochrane Library, Web of science and China National Knowledge Internet for articles evaluating the effectiveness of TPT in patients with RDs from inception through April 2023. Single rate meta-analysis and traditional meta-analysis were performed to compare the risk of ATB in RDs patients with or without TPT under various conditions. Single rate proportion, risk ratio (RR) and 95% confidence interval (CI) were calculated as the primary effect measure. Sensitivity analysis, risk of publication bias and article quality assessment were also completed.
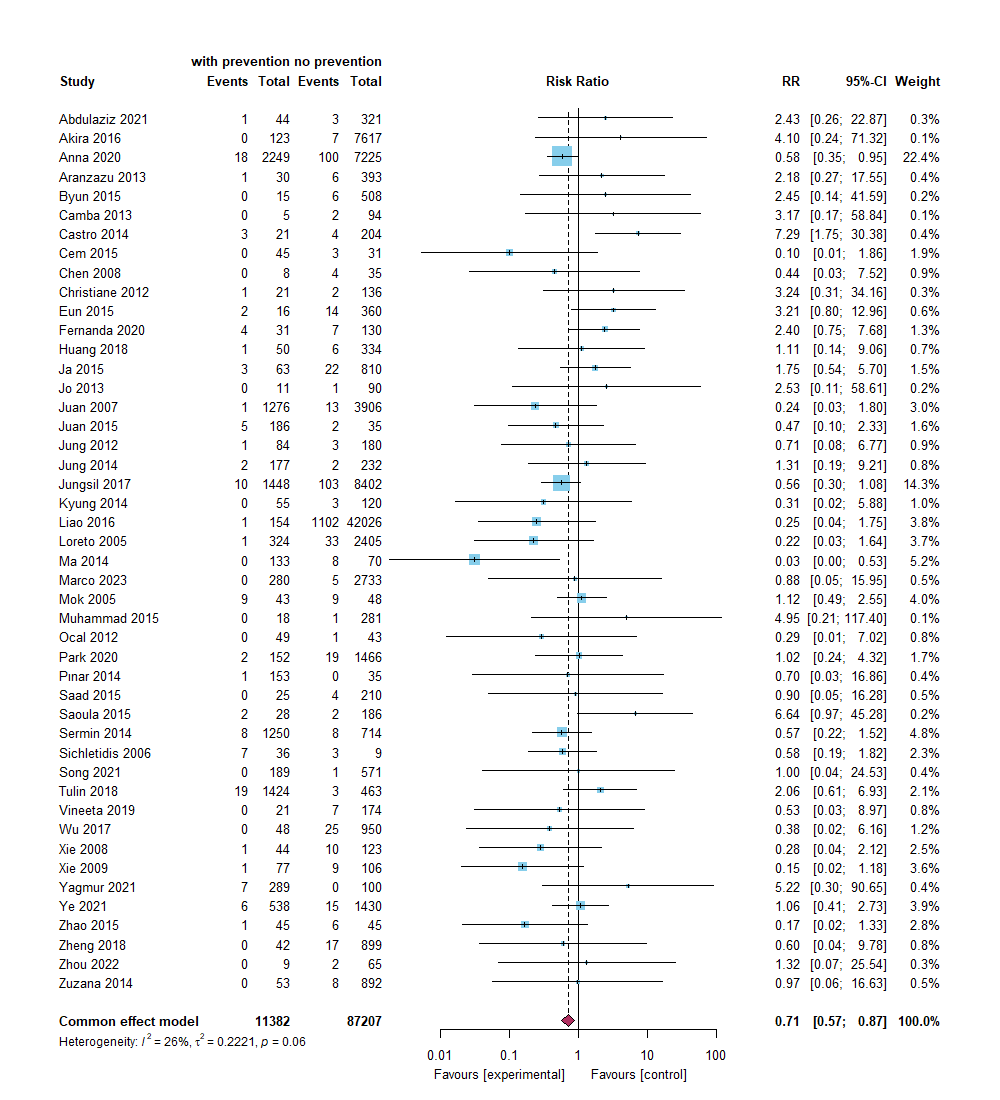
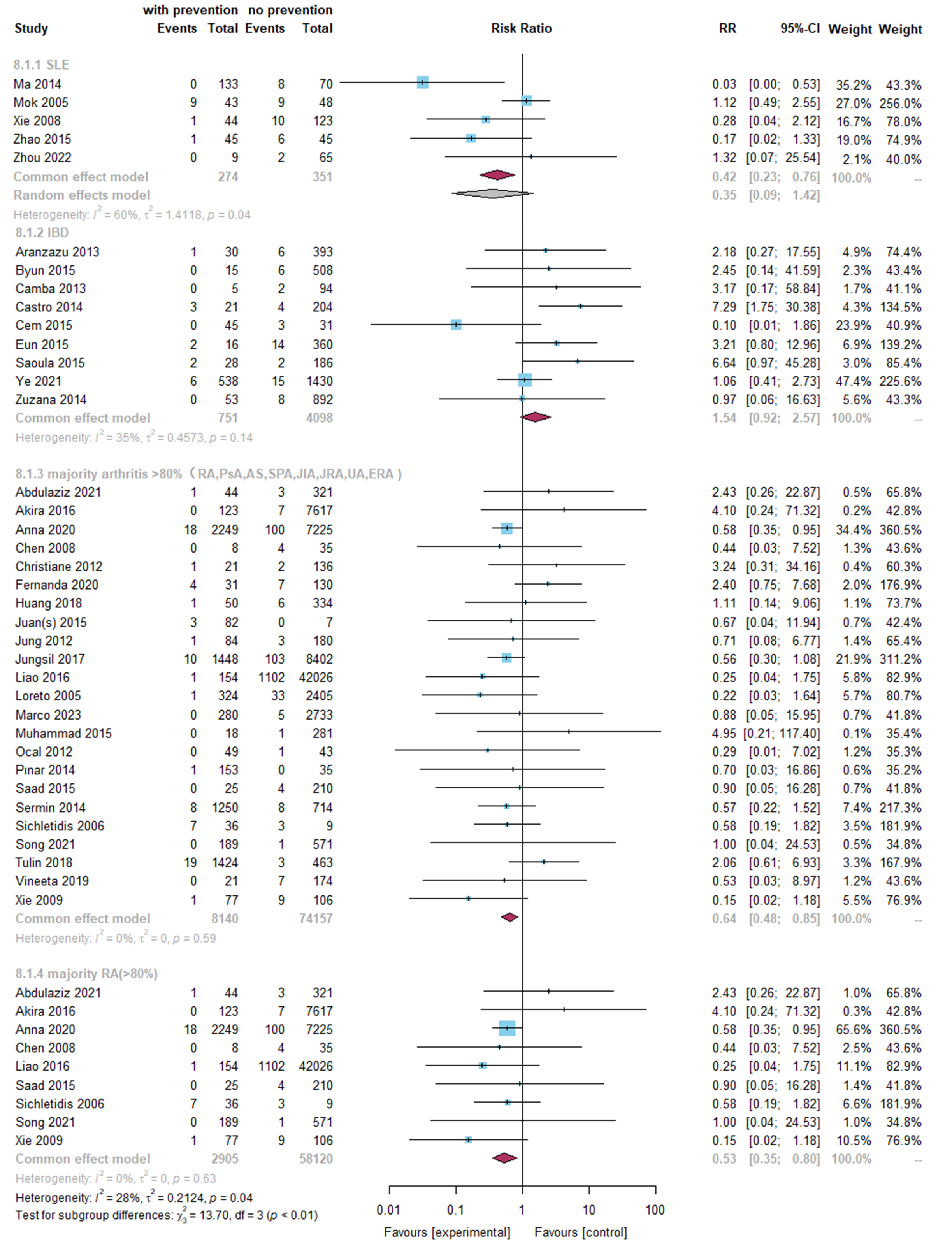
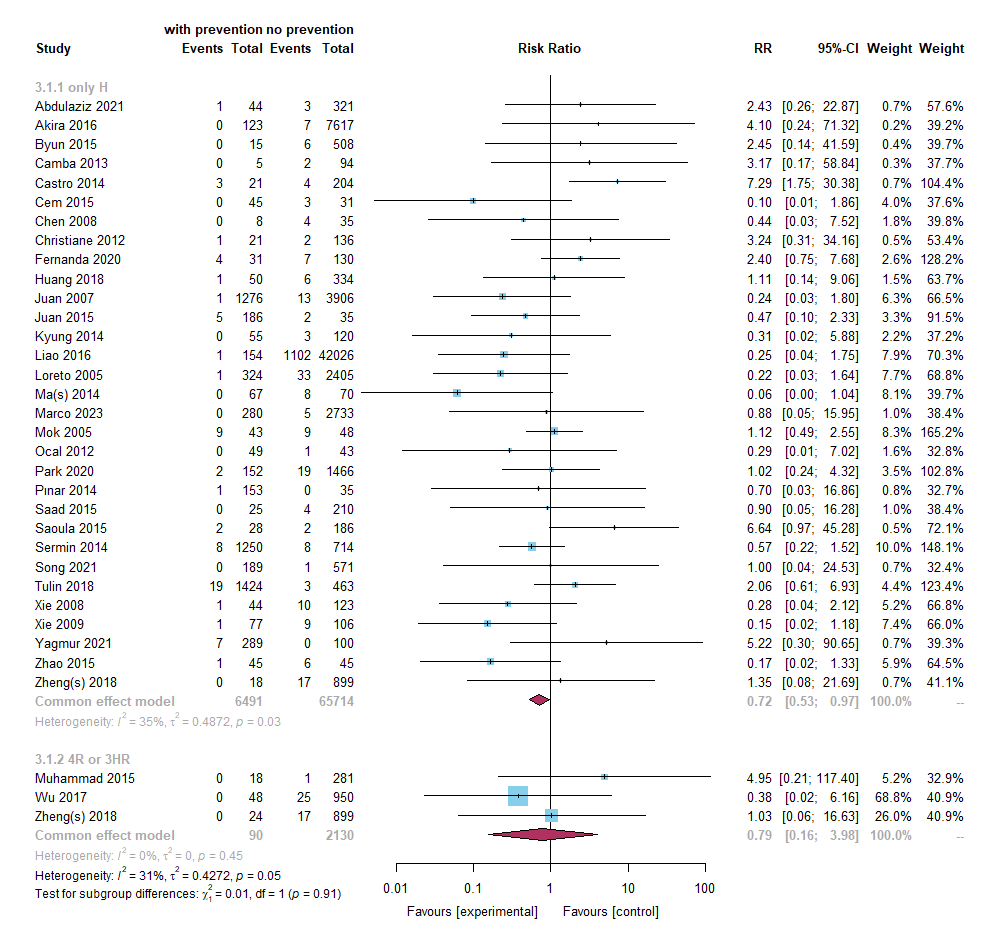
Results: Totally, 61 studies were included in single rate meta-analysis, and 46 studies were included in traditional meta-analysis. TB prevention decreased the overall risk of ATB in RDs patients (RR: 0.71, 95% CI: 0.57, 0.87). TB high burden countries (RR: 0.51, 95% CI: 0.32, 0.83) showed better effectiveness than other countries (RR: 0.76, 95% CI: 0.60, 0.96). Isoniazid preventive therapy (IPT) (RR: 0.72, 95% CI: 0.53, 0.97) was more effective. Furthermore, using IPT 9~12 months (RR: 0.52, 95% CI: 0.33, 0.82) was better than using IPT shorter than 9 months (RR: 1.32, 95% CI: 0.76, 2.27). Studies using rifamycin-containing TPT in RDs patients are limited, and its preventive effect is currently difficult to evaluate (RR: 0.79, 95% CI: 0.16, 3.98). When choosing LTBI screening method, tuberculin skin test (TST) combined with interferon gamma release assay (IGRA) (RR: 0.68, 95% CI: 0.50, 0.93) may be better than TST (RR: 0.96, 95% CI: 0.64, 1.43) or IGRA (RR: 0.68, 95% CI: 0.19, 2.46) alone. Not surprisingly, if RDs patients accepted biological agents during the treatment, it would decrease the effectiveness of TB prevention (RR: 0.79, 95% CI: 0.62, 0.99) than patients only received traditional treatment (RR: 0.44, 95% CI: 0.27, 0.73), but still significant. Noticeably, the effectiveness of TPT differed in different types of RDs: in patients with systemic lupus erythematosus (SLE), TPT seemed to be effective (fixed effect model RR: 0.42, 95% CI: 0.23, 0.76), and was also helpful in patients with immune mediated arthritis (RR: 0.64, 95% CI: 0.48, 0.85), but not in inflammatory bowel disease (IBD) patients (RR: 1.54, 95% CI: 0.92, 2.57).
Conclusion: This meta-analysis shows the evidence that TPT decreased the incidence of ATB in patients with RDs. TPT was more effective for patients in TB high burden country and not received biologic agent therapies. About the TPT options, using IPT over 9 months seemed to be better. Using IGRA combined with TST in LTBI screening strategy, RDs patients might benefit more.
To cite this abstract in AMA style:
Wang B, Chen S, Liu X, Zhang L. Effectiveness of Tuberculosis Preventive Treatment in Patients with Rheumatic Diseases: A Global Meta-analysis of Cohort Studies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/effectiveness-of-tuberculosis-preventive-treatment-in-patients-with-rheumatic-diseases-a-global-meta-analysis-of-cohort-studies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effectiveness-of-tuberculosis-preventive-treatment-in-patients-with-rheumatic-diseases-a-global-meta-analysis-of-cohort-studies/