Session Information
Date: Sunday, November 5, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: There is a lack of evidence on the effect of biologics in early treatment of psoriatic arthritis (PsA) patients (Pts). Benefit of concomitant use of DMARDs remains controversial in this indication.
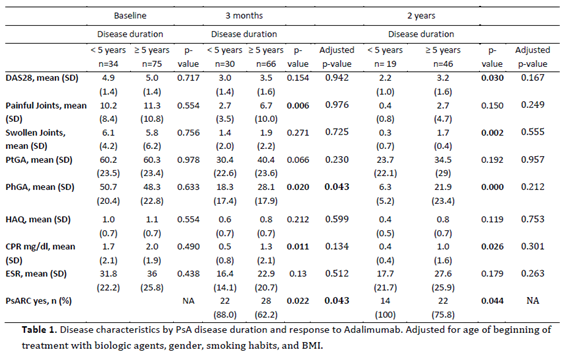
Methods: To compare clinical outcomes in patients with PsA starting adalimumab (ADA), with short and long disease duration and evaluate the potential effect of concomitant use of DMARDs or corticosteroids (CS), both on PsARC response and persistence on ADA.The analyses included adult PsA Pts who have been registered on Reuma.pt between June 2008 – June 2016 and have received ADA therapy for at least 3 months. PsARC, DAS28, tender and swollen joint count, ESR, CRP, PtGA, PhGA evaluated on a 10 cm VAS, and HAQ were compared between Pts <5 years of disease (early PsA) and those with ≥5 years of disease duration (late PsA) when starting ADA. Time to achieve PsARC response was estimated using Kaplan-Meier method, adjusted with Cox Regression with Efron method for ties with robust estimates of variance for baseline characteristics. Same analyses were repeated to compare patients with and without concomitant use of DMARDs or CS.
Results: We included 135 PsA patients who started ADA, 41 of them with early PsA. Pts with early PsA were younger, more frequently males, smokers, had significantly more hypertension. Overall, PsARC response was achieved by 72.9% of the Pts (88% early PsA vs 62.2% late PsA; p=0.022) at 3 months, by 85.4% of Pts at 24 months (100% early PsA vs 75.9% late PsA; p=0.044) after starting ADA. Patients with early PsA, achieved significantly less painful joints (2.7 vs 6.7; p=0.006), lower mean CRP (0.5 mg/dl vs 1.3 mg/dl, p=0.011) and PhGA (18.3 vs 28.1; p=0.020) at 3 months. In the long term, early PsA Pts showed less swollen joints (0.3 vs 1.7; p=0.030), lower PhGA (6.3 vs 21.9; p<0.001), CRP (0.4 mg/dl vs 1.0 mg/dl; p=0.026) and disease activity evaluated by DAS28 (2.2 vs 3.2; p=0.030). Early PsA Pts obtained PsARC response more rapidly than those with late PsA (3.8 and 7.4 months, respectively; p=0.008). Concomitant DMARDs, in the long term, showed clinical benefit (PsARC response at 2 years 88.3% vs 60.0%; p=0.044). Concomitant CS had no noticeable effect on PsARC response, over 2 years of follow-up. Survival on treatment with ADA was similar in the 2 groups and was not influenced by DMARD or CS therapy.
Conclusion: Patients with early PsA had greater chance of improvement after starting ADA, better functional outcome and achieved PsARC response more rapidly than patients with longer disease duration. Our results suggest that comedication with DMARDs may improve PsARC response in the long term.
To cite this abstract in AMA style:
Santos H, Eusébio M, Borges J, Gonçalves D, Ávila-Ribeiro P, Santos Faria D, Lopes C, Rovisco J, Águeda A, Nero P, Valente P, Cravo AR, Santos MJ. Effectiveness of Early Adalimumab Therapy in Psoriatic Arthritis Patients from Reuma.Pt [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/effectiveness-of-early-adalimumab-therapy-in-psoriatic-arthritis-patients-from-reuma-pt/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effectiveness-of-early-adalimumab-therapy-in-psoriatic-arthritis-patients-from-reuma-pt/