Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Medication adherence is a difficult charge in SLE. Up to 75% of lupus patients are non-adherent with hydroxychloroquine (HCQ). Pharmacy refill data measured by percent days covered (PDC) and HCQ levels are the main adherence measures used in SLE. Health literacy is an important culprit in non-adherence. Social cognitive behavior theories have been applied to understand the link between medication adherence and health literacy. Health literacy universal precautions refers to the steps that providers should take assuming all patients have difficulty comprehending health information. This study aimed to evaluate the effect of a provider led universal precautions intervention on medication adherence using indirect (PDC) and direct (HCQ blood level) measures of medication adherence and disease activity measures in a predominantly Hispanic, low SES, low health literacy, SLE population.
Methods: Data collected during a 6-month prospective intervention was compared with data from the 6-month pre-intervention period. Interventions based on the Agency for Healthcare Research and Quality universal health literacy precautions kit included 1) encouraging questions, 2) teach-back communication, and 3) brown-bag medication review. Analysis was performed using paired t-tests, comparing PDC (for HCQ, corticosteroids, immunosuppressants, and biologics), HCQ levels, and the hybrid SLEDAI (SLE disease activity index) scores from the pre- and post-intervention period. 60% of our cohort has limited health literacy.
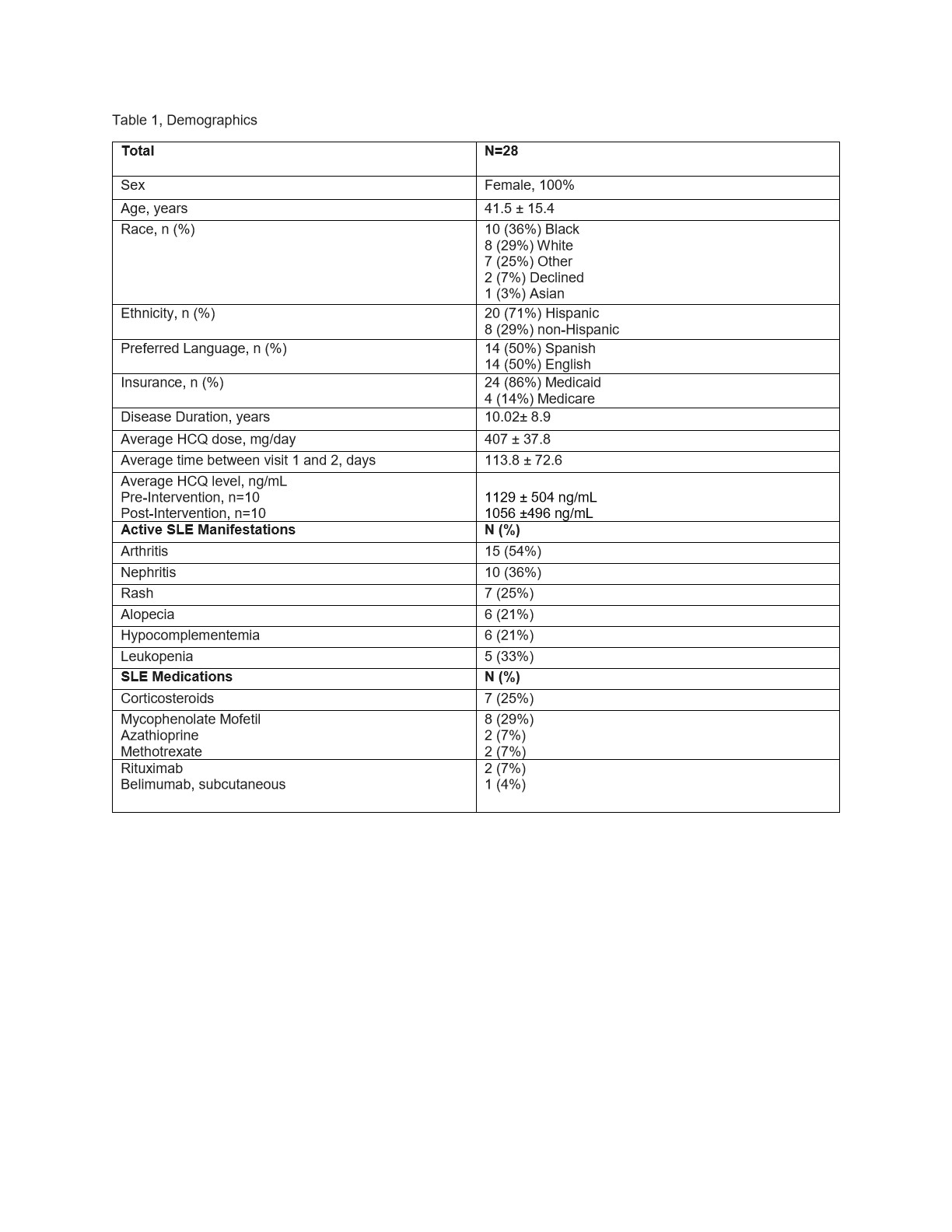
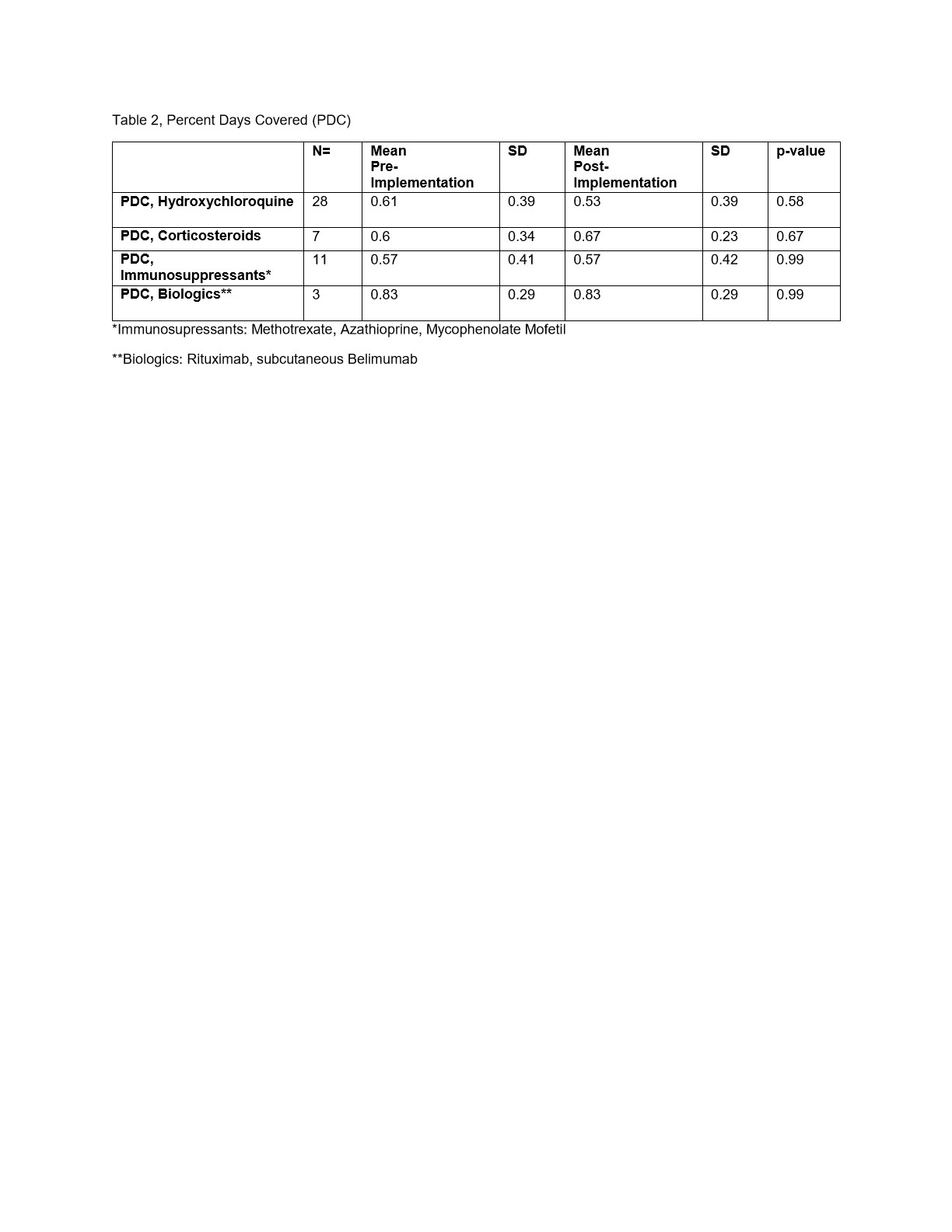
Results: The study included 28 women with SLE, mean age 43.1± 15.4 years, 71% Hispanic. 50% reported Spanish as preferred language, disease duration 10± 9 years. All patients had state funded health insurance (86% Medicaid, 14% Medicare) consistent with low SES. Patients reported taking 407 ± 37.8 mg of HCQ/day. Additionally, 25% of patients were prescribed corticosteroids, 11% biologics, and 43% immunosuppressants. During the intervention period, physicians completed 56 patient visits, 2 visits/patient, 113 ± 72 days apart. Median toolkit administration time was < 5 minutes. HCQ PDC decreased from 0.61 pre- to 0.53 post- intervention (p=NS); non-adherent < 0.80. HCQ blood levels were >1000 ng/mL both pre- and post-intervention, therapeutic HCQ > 500ng/ml. On an individual level, PDCs and blood levels were discordant. Two patients had high post intervention PDC ( >0.8) and sub-therapeutic blood levels. Prednisone adherence based on PDC increased from 0.6 to 0.67 (p=NS). Immunosuppressants PDC remained the same, 0.57. Biologics PDC was >0.8. SLEDAI decreased from 4.02 ± 4.31 to 2.88 ± 2.67 (p < 0.05).
Conclusion: In a population of predominantly Hispanic patients with SLE, low health literacy, and low SES, non-adherence was high across all medications except for biologics. The application of health literacy interventions provided conflicting results. This discordance could be due to differences in the recall periods; the recall period for PDC is 6 months, while HCQ levels only reflect weeks of adherence. The reasons for this discordance and non-adherence need to be further investigated and improved interventions to increase adherence should be sought.
To cite this abstract in AMA style:
Schmidt N, Gartshteyn Y, Kapoor T, Geraldino L, Khalili L, Askanase A. Effectiveness of a Provider Led Intervention on Medication Adherence in an Urban Lupus Clinic [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/effectiveness-of-a-provider-led-intervention-on-medication-adherence-in-an-urban-lupus-clinic/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effectiveness-of-a-provider-led-intervention-on-medication-adherence-in-an-urban-lupus-clinic/