Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Unlike primary antiphospholipid syndrome patients, most SLE patients with antiphospholipid antibodies are on one or more treatments for their SLE that might affect levels of their antiphospholipid antibodies. We examined the effect of prednisone and hydroxychloroquine on antiphospholipid antibodies in an SLE longitudinal cohort.
Methods: 943 SLE patients, who were tested for each anticardiolipin isotype (aCL IgG, IgM and IgA; INOVA) and lupus anticoagulant (dRVVT with further confirmatory testing) for at least 10 quarterly clinic visits, were included. We compared visits positive for antiphospholipid antibodies to visits negative for antiphospholipid antibodies, with respect to treatment, using conditional logistic regression and conditioning on the patient.
Results: The effect of prednisone on anticardiolipin and dRVVT > 45 (with further confirmatory testing) is shown in Table 1. The effect of hydroxychloroquine is shown in Table 2.
Conclusion: Prednisone does not reduce IgM or IgA isotypes of anticardiolipin, or lupus anticoagulant. These results explain why prednisone does not reduce thrombosis in SLE. Hydroxychloroquine, on the other hand, significantly reduces all antiphospholipid types except for the IgA isotype of anticardiolipin. This may explain why IgA isotypes are more common in SLE. It may also explain why hydroxychloroquine leads to only a 50% reduction in thrombosis, as IgA isotypes do confer some risk of thrombosis.
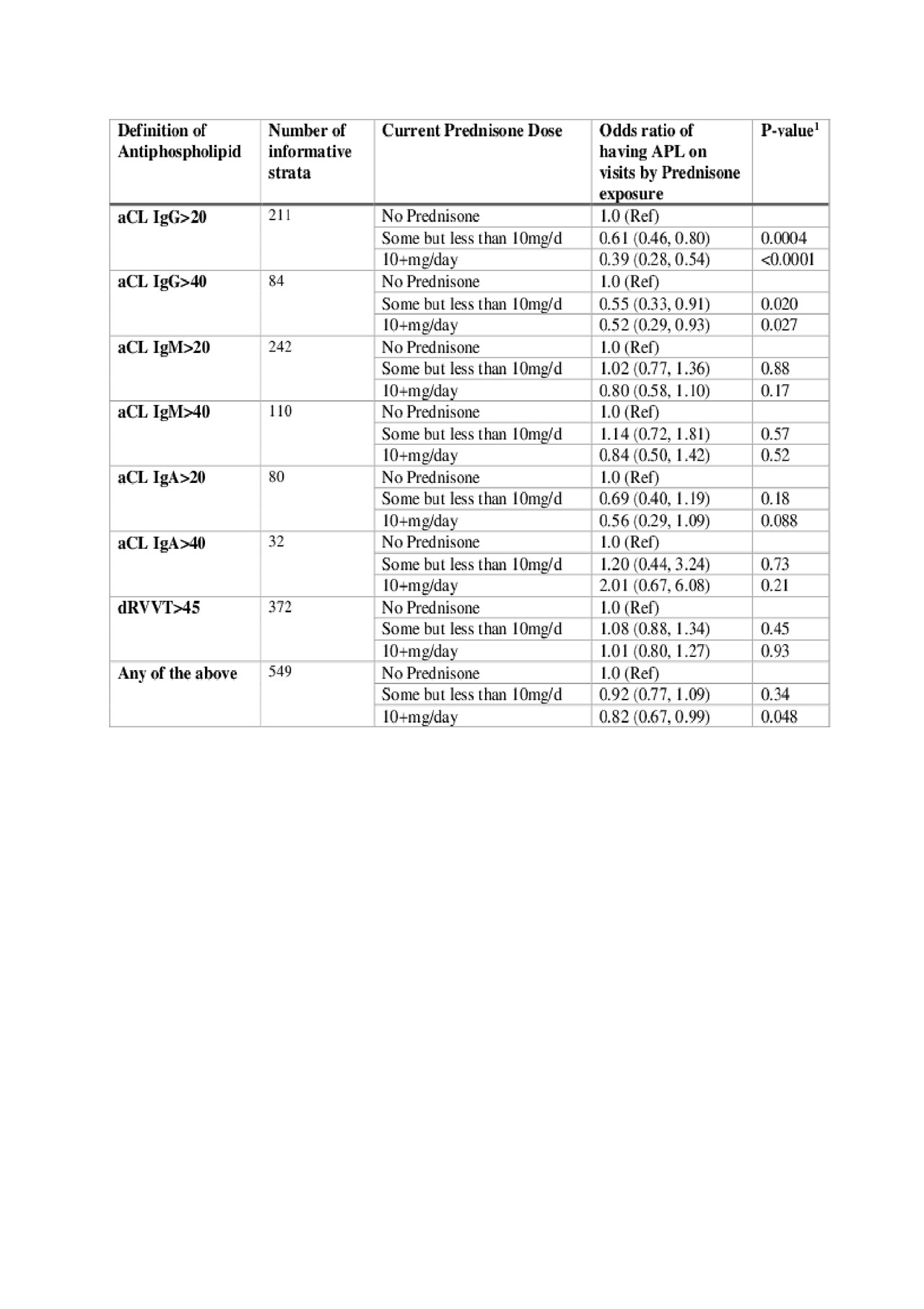
ACR 2019-Effect of Treatment on Antiphospholipid Antibodies in SLE-Table1
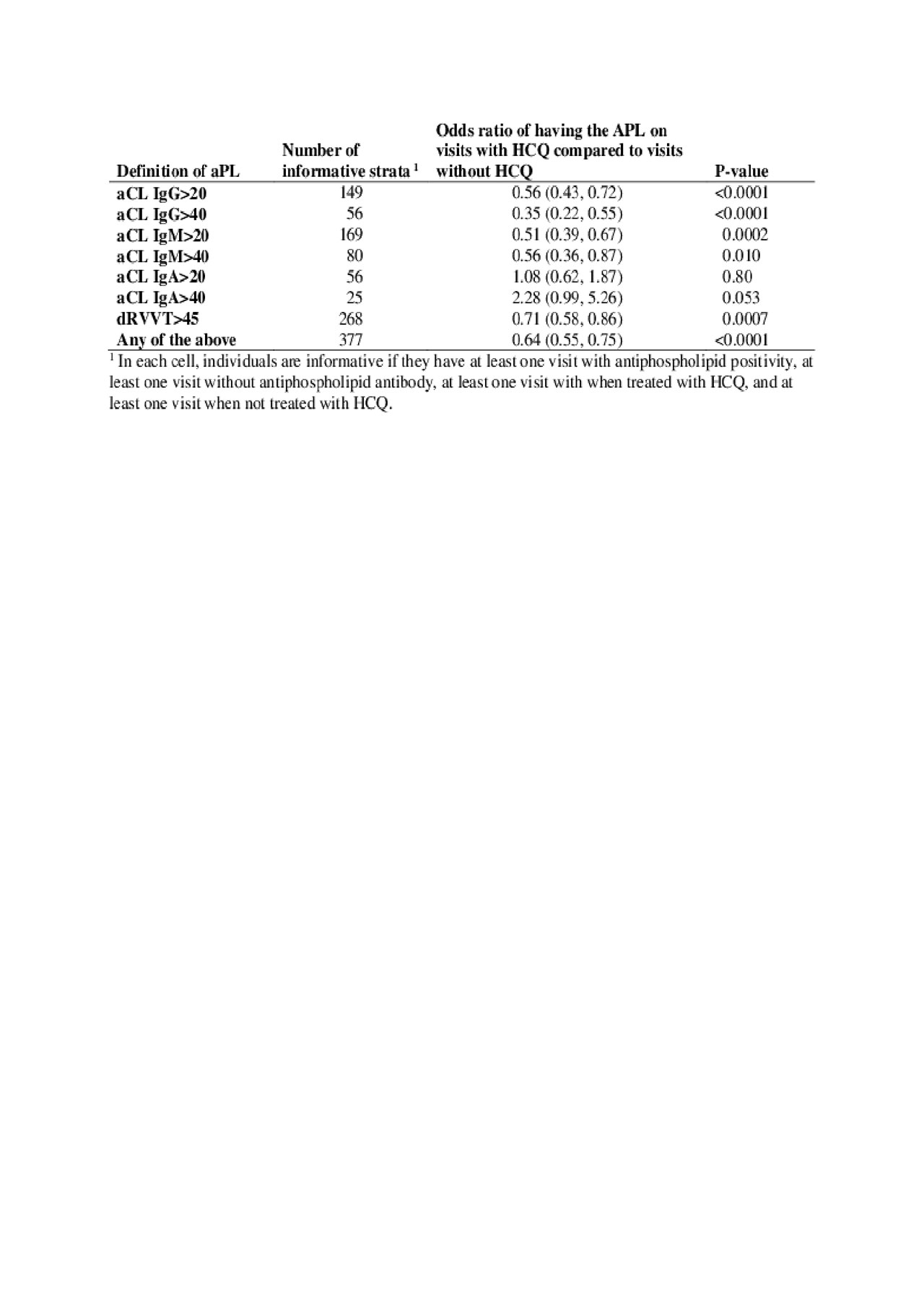
ACR 2019-Effect of Treatment on Antiphospholipid Antibodies in SLE-Table2
To cite this abstract in AMA style:
Petri M, Magder L, Goldman D. Effect of Treatment on Antiphospholipid Antibodies in SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/effect-of-treatment-on-antiphospholipid-antibodies-in-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-treatment-on-antiphospholipid-antibodies-in-sle/
