Background/Purpose:
Recent randomized controlled trials in rheumatoid arthritis (RA) patients have determined that a strategy of first adding the two Disease Modifying Anti-Rheumatic Drugs (DMARDs) sulfasalazine and hydroxychloroquine to methotrexate (a combination known as Triple Therapy) is neither inferior nor less safe than first adding anti-TNF drugs in patients with active disease despite methotrexate. The implication is that inexpensive triple therapy should be initiated prior to expensive biologic therapy. In this study we examine historical biologic and Triple Therapy use in British Columbia (BC), Canada over the past 10 years. We sought to estimate the potential savings in expenditures if Triple Therapy use had been more prevalent, and project potential future cost-savings.
Methods:
We examined a population-based cohort of all BC patients with a rheumatologist diagnosis of RA identified from administrative data. We selected prevalent RA cases who used a biologic for the first time between 2001 and 2010 and examined their prior DMARD history from prescription billing data. For each year, we calculated the proportion of patients that had used Triple Therapy, the average drug prices, and the average duration patients remain on Triple Therapy. Since not all patients can use Triple Therapy, we conducted a series of scenarios which estimated the cost that would have been saved if a higher proportion of patients had used Triple Therapy.
Results:
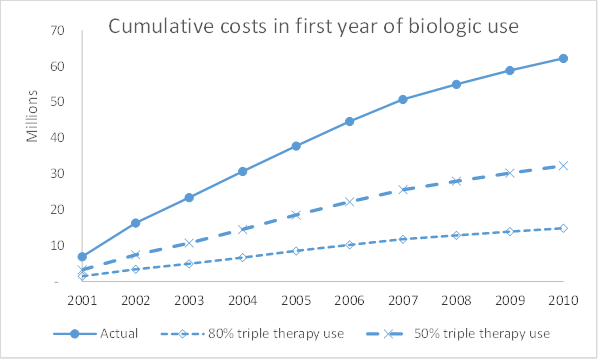
In total, we examined 2726 RA patients who started their first biologic over the time period. Triple therapy use prior to biologic therapy has increased over time, from 15.2% in 2001 to 24.4% in 2010. The average duration patients remained on triple therapy was 1.13 years. Of the $62million spent on patients first year of biologics, a scenario where 80% of patients would have received triple therapy instead would have resulted in cost savings to BC of $47.3 million over the 10 year period (figure 1). Assuming similar patterns of triple therapy use across Canada, projections suggest future cost-savings of over $12 million per year if triple therapy is used in 80% of patients prior to biologic use. Various sensitivity analyses are performed.
Conclusion:
Higher utilization of Triple Therapy will require a willingness for rheumatologists to prescribe it, and a willingness for patients to use it. With the benefit of hindsight, higher use of Triple Therapy prior to biologic initiation would have released a substantial amount of pharmaceutical spending to alternative treatments. Importantly, with less than 25% of patients currently receiving triple therapy prior to a biologic, there is still a considerable potential for future savings. Strategies such as academic detailing and patient decision aids may be good investments if they can change treatment choices.
Disclosure:
N. Bansback,
None;
D. V. Lacaille,
None;
D. Guh,
None;
K. Shojania,
None;
A. H. Anis,
Pfizer Inc,
2,
Antares, Pfizer, Abbvie,
5.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/economic-implications-for-policies-regarding-triple-therapy-use-in-patients-with-rheumatoid-arthritis/