Session Information
Date: Saturday, November 6, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster I: Impact (0225–0240)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Fatigue is a complex symptom affecting physiological, psychological, and social factors and is commonly seen in psoriatic arthritis (PsA). The objectives of this study were to evaluate healthcare resource utilization and costs associated with fatigue among patients with PsA in the United States.
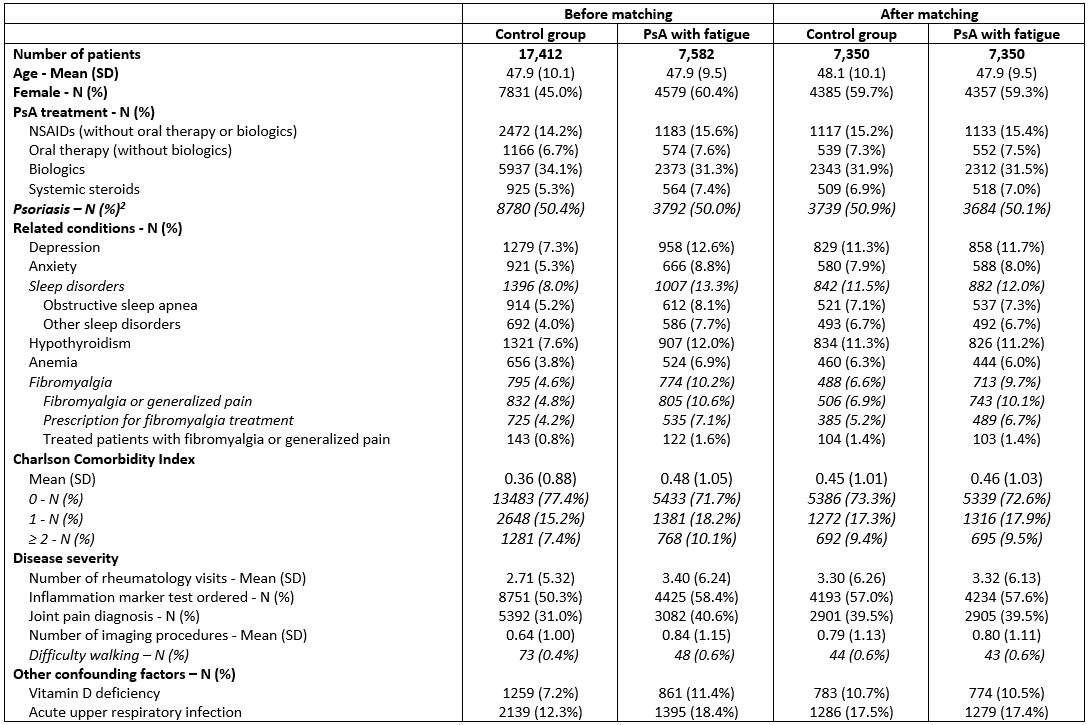
Methods: The IBM® MarketScan® Commercial Database was used to identify adult patients with PsA between 2009 and 2019. Patients with ≥ 2 diagnoses for PsA ≥ 30 days apart were included. Patients with fatigue (i.e., cases) had ≥ 1 fatigue diagnosis after their initial PsA diagnosis, and the first fatigue diagnosis was defined as the index date. Controls were PsA patients who had no fatigue diagnoses during the study period; their index date was defined using the case’s median time from initial PsA to the first fatigue diagnosis. Patients had continuous enrollment from ≥ 6 months before their initial PsA diagnosis (baseline period) to ≥ 12 months after the index date (follow-up period). Patients with comorbid rheumatoid arthritis, ankylosing spondylitis, Crohn’s disease, or ulcerative colitis during the study period were excluded from the analyses. Controls were matched 1:1 to patients with PsA and fatigue based on propensity scores that balanced age, gender, year of initial PsA diagnosis, PsA treatment, related conditions, the Charlson Comorbidity Index, variables associated with PsA disease severity, vitamin D deficiency, and respiratory infection (Table 1). Healthcare resource utilization and costs (in 2019 USD) were evaluated during follow-up.
Results: Fatigue was present among 30% of included patients with PsA. 7,350 patients with fatigue were matched to the control group (Table 1). The average age at baseline was 48 years and 59% were female. Average annual all-cause healthcare costs per patient were $26,102 and $34,344 for the control group and patients with fatigue, respectively (p< 0.0001). The costs were greater among patients with fatigue due to greater inpatient costs (controls: $2,046, fatigue: $3,959), outpatient medical costs (controls: $7,058, fatigue: $11,182), and outpatient pharmacy costs (controls: $16,998, fatigue: $19,203) (Figure 1). Across all categories of healthcare resources, utilization was greater among patients with PsA and fatigue than the control group (Table 2). Patients with PsA and fatigue had significantly more physician office visits than controls during follow-up (average of 11.4 and 8.0, respectively, p< 0.0001).
Conclusion: PsA patients with fatigue incurred significantly greater healthcare costs and resource utilization than patients without fatigue. Effective treatments that help reduce fatigue among patients with PsA may improve patient outcomes including decreased healthcare costs. Further research is warranted to better understand what is driving these greater costs.
To cite this abstract in AMA style:
Merola J, Yang F, Dennis N, Peterson S, Lin I, Wang Y, Chakravarty S, Quenéchdu A, Shawi M, Fischer C, Husni E. Economic Burden of Fatigue Among Patients with Psoriatic Arthritis – a Retrospective Study Using Claims Data, 2009-2019 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/economic-burden-of-fatigue-among-patients-with-psoriatic-arthritis-a-retrospective-study-using-claims-data-2009-2019/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/economic-burden-of-fatigue-among-patients-with-psoriatic-arthritis-a-retrospective-study-using-claims-data-2009-2019/