Session Information
Title: Systemic Sclerosis, Fibrosing Syndromes, and Raynaud’s - Clinical Aspects and Therapeutics II
Session Type: Abstract Submissions (ACR)
Background/Purpose: The leading causes of death in systemic sclerosis (SSc) are pulmonary arterial hypertension (PAH) and interstitial lung disease (ILD). Use of PAH therapy in patients with both SSc-PAH and ILD is controversial and may not improve survival (1). This study investigates transplant-free survival in patients with SSc-PAH, both with and without ILD, treated aggressively with PAH therapies.
Methods: All SSc patients who had a right heart catheterization (RHC) diagnostic for PAH (mean pulmonary artery pressure (mPAP) greater than or equal to 25 mm Hg, pulmonary capillary wedge pressure (PCWP) less than or equal to 15 mm Hg, pulmonary vascular resistance (PVR) greater than or equal to 240 dynesxsecond/cm5), between 2001-2012 were enrolled. ILD was defined as greater than 30% disease extent on high-resolution computed tomography (HRCT) or when disease extent 10-30%, forced vital capacity less than 70%. Kaplan-Meier and Cox proportional hazards models were used to analyze survival and identify prognostic variables.
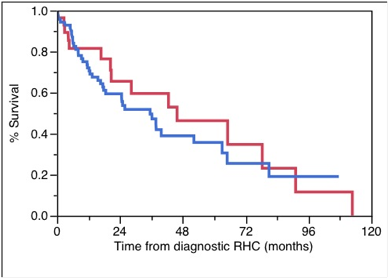
Results: Of the 99 patients with SSc-PAH, 71 also had ILD. Patients with PAH+ILD were younger than patients with PAH alone (Mean 55 years vs. 60 years, respectively, p=0.07) and a smaller percentage were woman (70% vs. 93%, respectively, p=0.02). SSc type/disease duration, ethnicity, co-morbidities, hemoglobin, creatinine, mPAP, PCWP, PVR, use of supplemental oxygen, and six-minute walk distance were similar between patients with PAH alone and PAH+ILD. Twenty-four percent of all patients started prostacyclin therapy within 6 months of the RHC, while 24% started prostacyclin therapy after 6 months of the RHC. The 1-, 2-, 3-year survival estimates were 72%, 59%, 50%, and 82%, 66%, 60%, for the PAH+ILD and PAH alone groups, respectively, p=0.5 (Figure 1). In the multivariate model, after controlling for potentially confounding variables, male gender (hazard ratio 0.6, p=0.008) and prostacyclin therapy initiation within 6 months of the RHC (hazard ratio 1.4, p=0.007) were the only factors significantly associated with transplant-free survival.
Conclusion: Survival of SSc-PAH and ILD has improved compared with historical series (1); this may in part be due to aggressive use of prostacyclin therapy.
References:
(1) Le Pavec J, et al. Arthritis Rheum 2011;63:2456.
Figure 1. Kaplan-Meier survival curves demonstrating no significant difference in transplant-free survival for SSc-PAH patients with ILD (blue line) and without ILD (red line) (Log rank p-value 0.5).
Disclosure:
E. Volkmann,
None;
R. Saggar,
Gilead,
9,
United Therapeutics,
9,
Actelion Pharmaceuticals US,
9;
B. Torres,
None;
L. Yoder,
None;
R. Elashoff,
None;
R. Saggar,
Actelion Pharmaceuticals US,
9,
United Therapeutics,
9,
Gilead,
9;
H. Agrawal,
None;
N. Borazan,
None;
S. Thomas,
None;
D. Furst,
AbbVie,
2,
Actelion Pharmaceuticals US,
2,
Amgen,
2,
BMS,
2,
Gilead,
2,
GlaxoSmithKline,
2,
NIH,
2,
Novartis Pharmaceutical Corporation,
2,
Pfizer Inc,
2,
Roche Pharmaceuticals,
2,
Genentech and Biogen IDEC Inc.,
2,
UCB,
2,
AbbVie ,
8,
Actelion Pharmaceuticals US,
8,
UCB,
8.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-use-of-prostacyclin-therapy-improves-transplant-free-survival-in-patients-with-systemic-sclerosis-related-pulmonary-arterial-hypertension-plus-interstitial-lung-disease/