Session Information
Date: Sunday, October 21, 2018
Title: Pediatric Rheumatology – Clinical Poster I: Lupus, Sjögren’s Disease, and Myositis
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Daily oral prednisone has been the main therapy in juvenile dermatomyositis (JDM), and combination therapy with methotrexate (MTX) introduced soon after diagnosis has been increasingly used. There have been few randomized studies to provide evidence for therapeutic choices in JDM. We therefore evaluated effects of initial therapies on treatment outcomes using propensity score analysis in a large North American JDM registry.
Methods: We examined outcomes associated with 3 treatments used in the first 3 months after diagnosis in 286 JDM patients: high (≥2 mg/kg/d) vs. low daily prednisone dose; pulse intravenous methylprednisolone (IVMP) vs. none; MTX vs. none. The 4 outcomes, achievement of half of the initial prednisone dose, prednisone discontinuation, treatment escalation at 12 and 24 months, and development of calcinosis, were evaluated by Cox proportional hazards and logistic regression. We accounted for differences in use of initial therapies by creating propensity score models that were matched 1:1 for patients with and without each therapy. Differences in the propensity score model covariates were examined by Chi-square and Wilcoxon rank sum tests. Initial hazard models did not include the use of other medications, while final models adjusted for duration of other medications received.
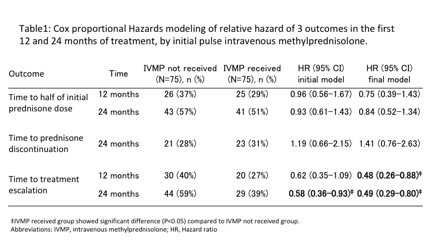
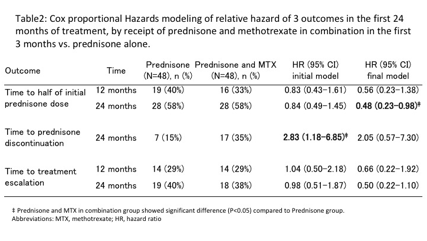
Results: Of 286 patients, 169 received high dose prednisone, 83 received IVMP, and 90 received MTX in the first 3 months. The propensity score models had good fit, indicated by reduced model AIC values compared to intercept only models, and each of the covariates was balanced between treatment groups within each of the propensity score quartiles. High doses prednisone had no effect on the likelihood of achieving the 3 treatment outcomes compared to lower doses of prednisone. Patients receiving initial pulse IVMP were less likely to have a treatment escalation at 12 and 24 months compared to those not receiving pulse IVMP (Table1). Patients receiving prednisone/MTX in combination in the first 3 months were more likely to achieve prednisone discontinuation at 24 months in a model without adjustment for other medications received (Table2). These 3 initial therapies had no association with the development of calcinosis at ≥ 24 months.
Conclusion: Initial pulse IVMP therapy and prednisone in combination with MTX in the first 3 months of treatment are associated with reduced requirements for future treatment in JDM patients. There was no association of initial prednisone dose with these outcomes. Pulse IVMP and MTX in combination with prednisone are recommended in the early treatment of JDM patients.
To cite this abstract in AMA style:
Kishi T, Wilkerson J, Smith M, Bayat N, Henrickson M, Lang B, Passo M, Miller FW, Ward M, Rider LG. Early Treatment with Intravenous Pulse Methylprednisolone or Methotrexate Is Associated with Decreased Medication Requirements at 12 and 24 Months in Patients with Juvenile Dermatomyositis: A Propensity Score Analysis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/early-treatment-with-intravenous-pulse-methylprednisolone-or-methotrexate-is-associated-with-decreased-medication-requirements-at-12-and-24-months-in-patients-with-juvenile-dermatomyositis-a-propensi/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-treatment-with-intravenous-pulse-methylprednisolone-or-methotrexate-is-associated-with-decreased-medication-requirements-at-12-and-24-months-in-patients-with-juvenile-dermatomyositis-a-propensi/