Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
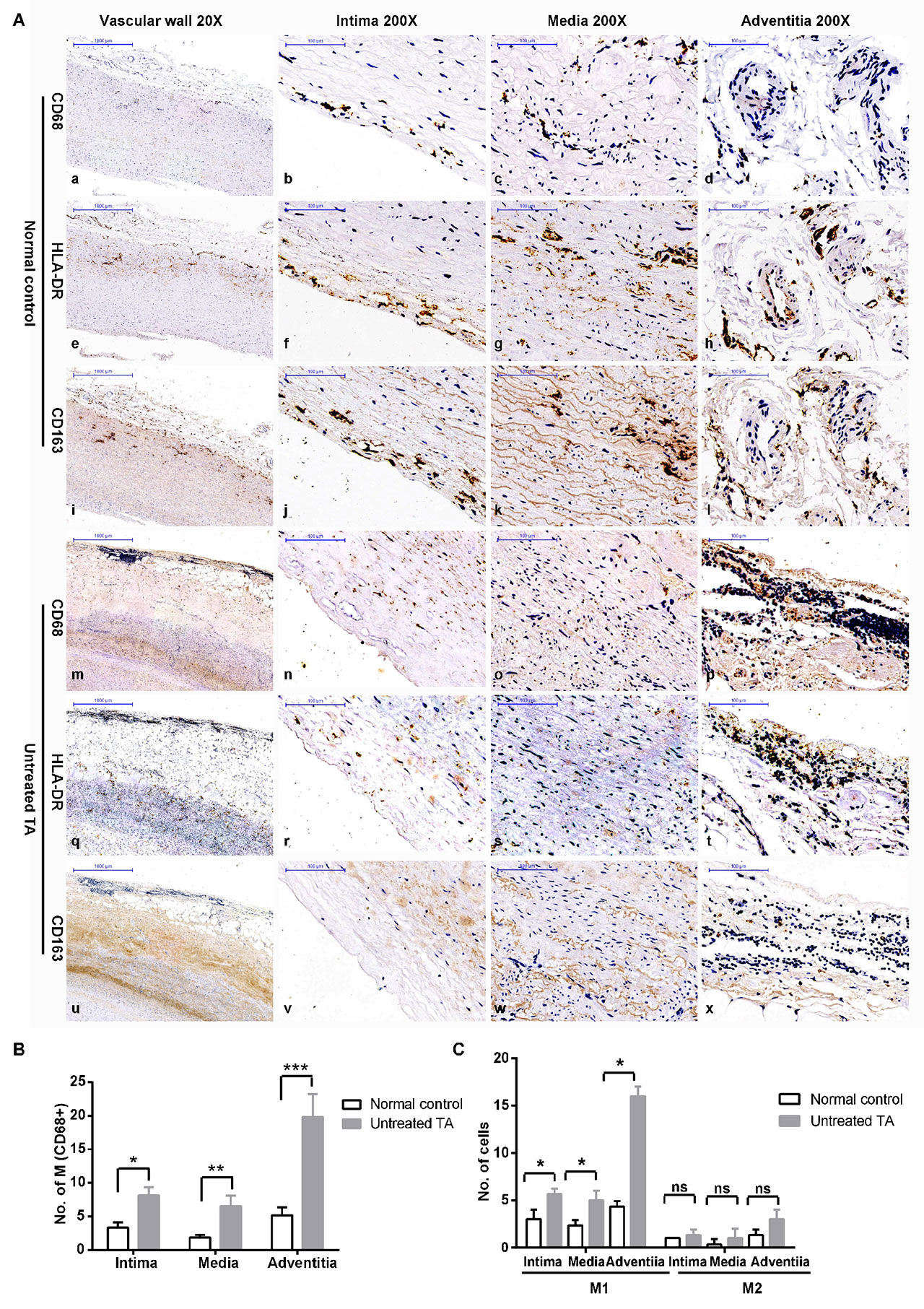
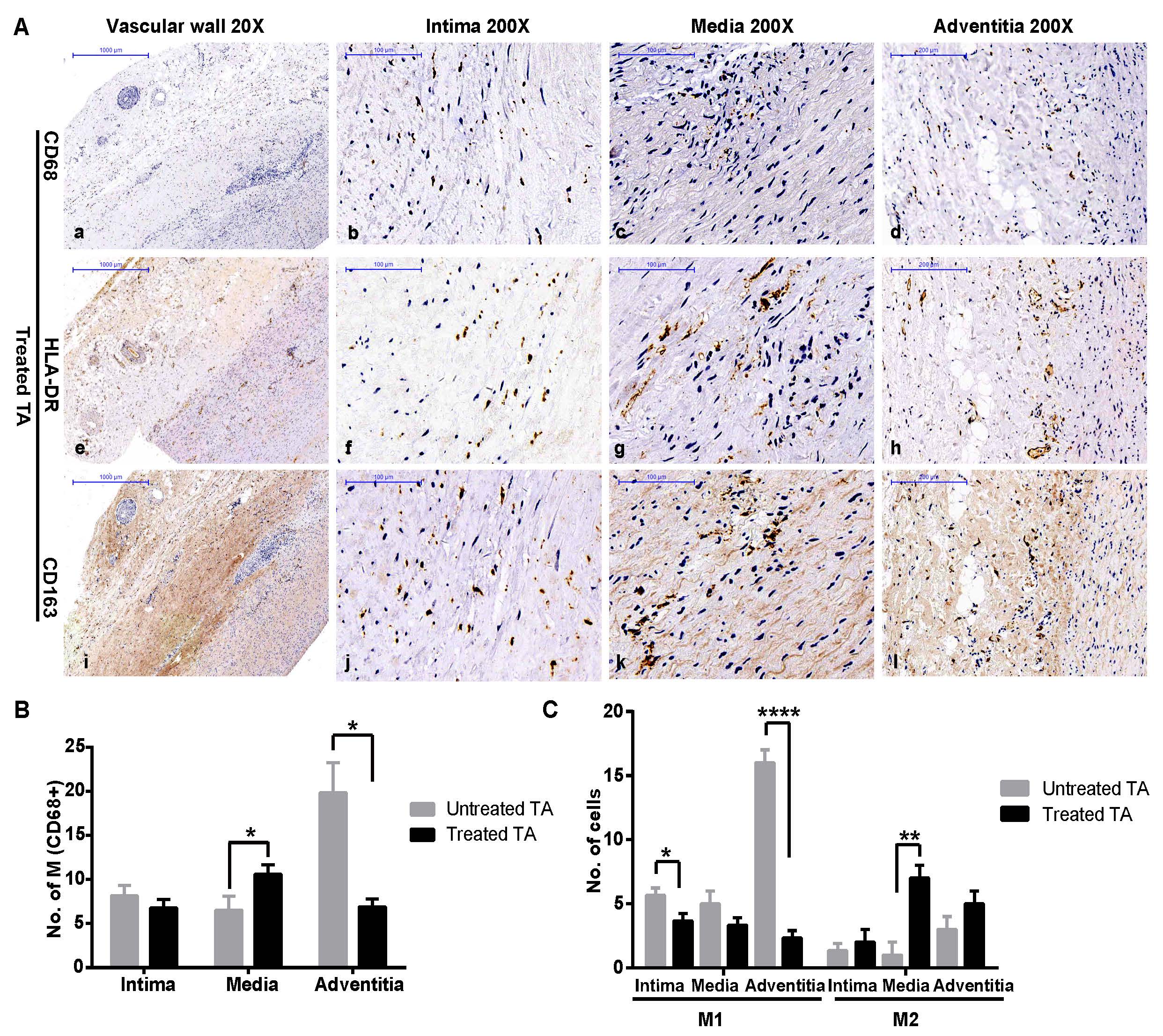
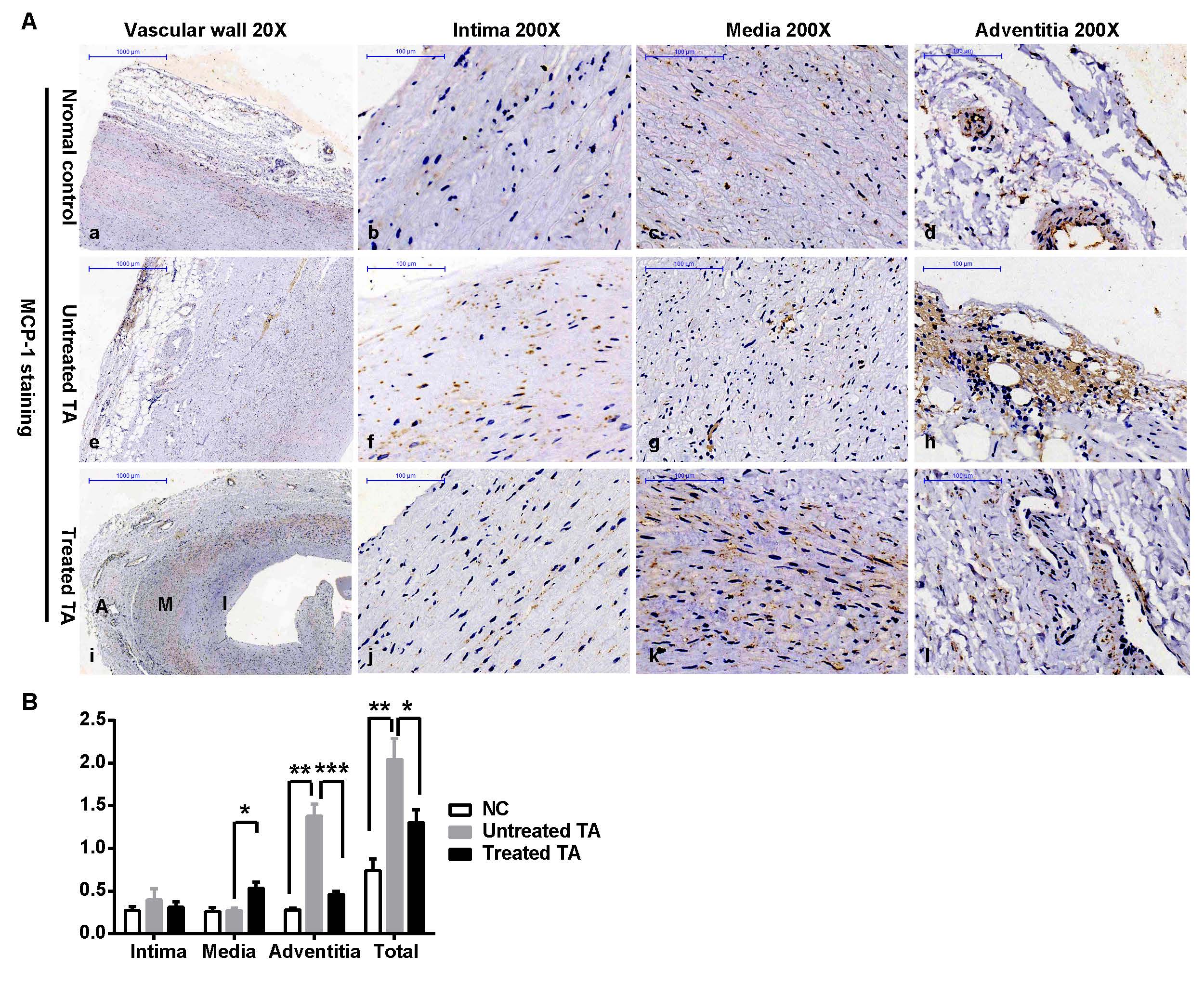
Background/Purpose: Takayasu arteritis (TA) is a chronic inflammatory disease characterized by arterial vascular fibrosis. Type I (M1) and type II (M2) macrophages play very important roles in the development of TA, and monocyte chemotactic protein-1 (MCP-1) has also been implicated in TA. However, the roles and interactions of these three factors with each other and with the current therapeutic agents for TA are unclear. Therefore, in the current study, we investigated the M1 and M2 profile in the vascular tissue of TA patients and detected the concentration of monocyte chemotactic protein-1 (MCP-1) in vascular tissue and peripheral blood before and after treatment.
Methods: This study included 8 untreated TA patients, 7 treated patients and 4 controls who provided vascular tissue specimens, as well as 38 treatment-naïve patients and 28 healthy controls who provided their serum samples before and after treatment (only 19 TA samples were obtained after treatment). The treatment strategy was prednisone combined with immunosuppressants. Immunohistochemical staining for M1 and M2 markers and MCP-1 was performed in the vascular tissue samples. The serum level of MCP-1 was detected by ELISA. Disease activity was evaluated by the Kerr activity score.
Results: M1 macrophages were more prominent in the acute (pro-inflammatory) stage of TA and in naïve patients, while M2 macrophages were more prominent in the chronic (pro-fibrotic) stage and in treated patients. This pattern was also observed in MCP-1 expression. Macrophages and MCP-1 showed increased levels in vascular tissue (mainly in the adventitia), along with an increase in peripheral MCP-1, in the treatment-naïve patients. In contrast, in the patients who had received 6 months of treatment, both the macrophage and MCP-1 (vascular adventitia and peripheral) levels were decreased. In the vascular media from treated patients, an increase in MCP-1 levels and M2 infiltration was observed. Furthermore, peripheral MCP-1 was correlated Kerr activity score (Rho = 0.50, P = 0.002) and peripheral IL-6 levels (Ro = 0.55, P < 0.001).
Conclusion: In the vascular wall, M1 and M2 distribution is dynamic and is closely associated with MCP-1 expression, which is increased in the serum and vascular tissue of TA patients. The current treatment strategies do not target M2 infiltration, as a result of which fibrosis is aggravated. Thus, more efficacious treatment strategies that target both M1 and M2 should be used. Further, the serum level of MCP-1 may prove to be a useful indicator of disease stage and treatment efficacy in the future.
To cite this abstract in AMA style:
Kong X, Xu M, Cui X, Ma L, Chen H, Ma L, Jiang L. Dynamic Distribution and Phenotype Shift from M1 to M2 of Macrophages in Vascular Lesions of Naïve and Treated Patients with Takayasu Arteritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/dynamic-distribution-and-phenotype-shift-from-m1-to-m2-of-macrophages-in-vascular-lesions-of-naive-and-treated-patients-with-takayasu-arteritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dynamic-distribution-and-phenotype-shift-from-m1-to-m2-of-macrophages-in-vascular-lesions-of-naive-and-treated-patients-with-takayasu-arteritis/