Session Information
Date: Sunday, November 12, 2023
Title: (0510–0542) Spondyloarthritis Including Psoriatic Arthritis – Treatment: AxSpA Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In the management of axial spondyloarthritis (axSpA), treatment intensification (TI) is recommended in patients with high disease activity (HDA). However, in practice, in most patients who are in an HDA state, treatment is not changed. Possibly, other factors than disease activity, such as disease impact and acceptability of current health state, drive the decision for TI. Our objective was to explore which patient- and disease-related determinants are associated with TI in axSpA patients with HDA.
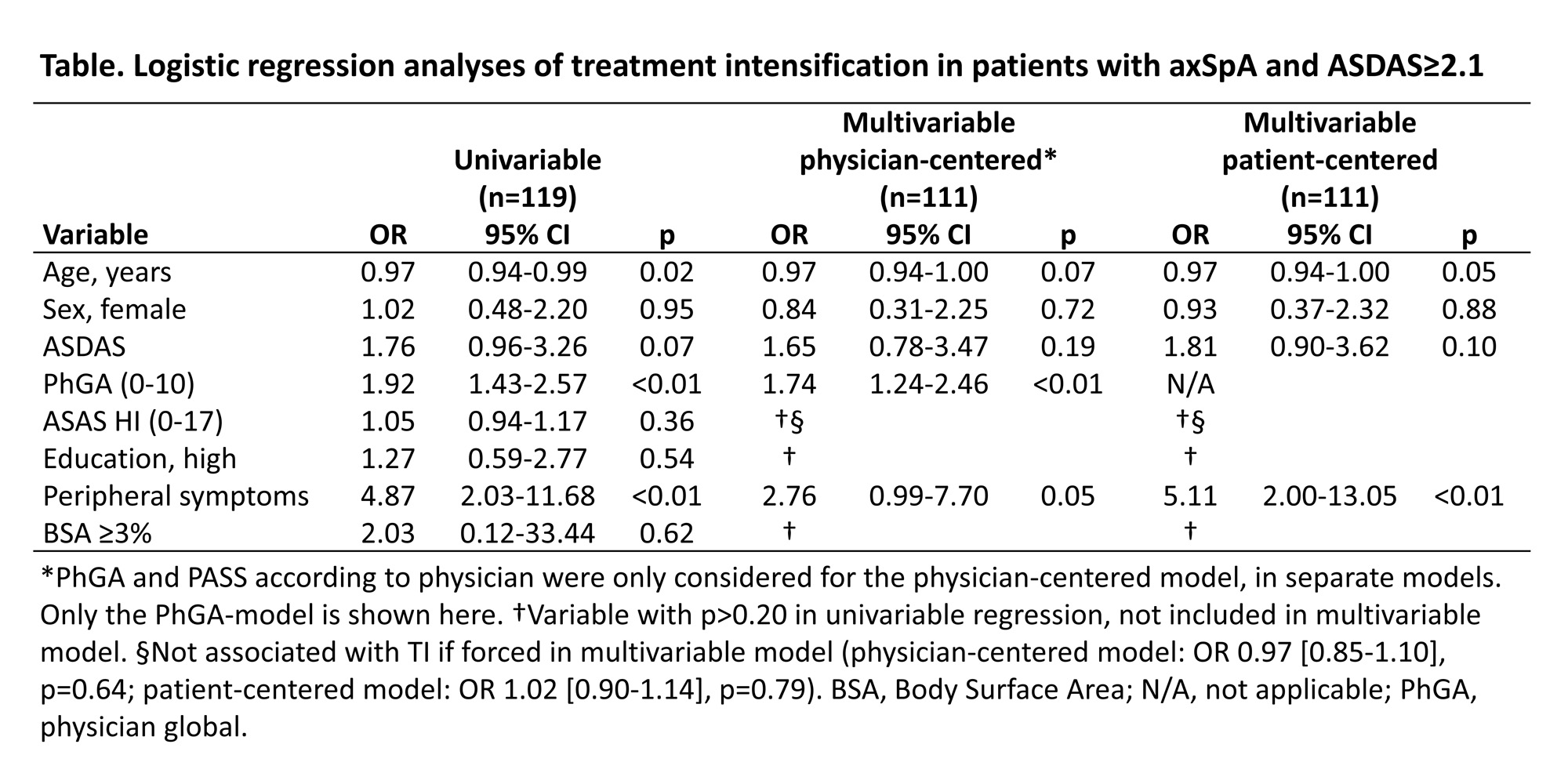
Methods: In this cross-sectional observational study, one time point per patient was used from SpA-Net, a multicentre registry for SpA. Only patients in an HDA state (defined as Ankylosing Spondylitis Disease Activity Score [ASDAS]≥2.1) were included. The outcome (TI) was defined as 1) a higher dose or shorter interval of the same drug, 2) a switch of the current drug to another drug or 3) addition of a new drug to the current treatment regime; and only due to inefficacy of the current treatment. Only anti-inflammatory drugs (NSAIDs, conventional synthetic/biologic/targeted synthetic DMARDs [cs/b/tsDMARDs], corticosteroids) were considered. Primary determinants were ASDAS, Assessment of SpondyloArthritis international Society Health Index (ASAS HI) and physician global (PhGA). Education, peripheral symptoms and skin involvement were also considered as determinants. Acceptable symptom state according to patient (PASS-patient) or physician (PASS-physician) were included in sensitivity analyses. The association between determinants and TI was investigated with multivariable logistic regression. Both physician-centered and patient-centered models were generated.
Results: In total, 119 patients in an HDA state were included. Mean age was 50.4 (SD 13.5) years, symptom duration 20.1 (13.2) years and 65 patients (54.6%) were female. The majority were currently in an acceptable state (PASS-patient 57.1%, PASS-physician 66.7%). TI was conducted in 40 patients (33.6%). Patients in which TI was not applied were older, less often employed and more likely to be on biological treatment at time of ASDAS≥2.1. In physician-centered regression analyses, the physician-based determinants were very strong and independent drivers for TI (ORPhGA = 1.74 [95%CI 1.24-2.46]; ORPASS-physician = 27.0 [4.18-174.0]) while patient-based determinants (ASDAS, ASAS HI, education) were not associated with TI (Table). In patient-centered regression analyses, only peripheral symptoms were associated with TI. PASS-patient was not associated with TI in any of the models (OR = 1.22 [0.34-4.45] when added to the patient-centered model).
Conclusion: In practice, treatment is intensified in only a minority of patients with axSpA and HDA. Physician-centered factors seem to be driving this decision to change treatment, independently of (ASDAS-based) disease activity. Further research is needed to better understand these decisions.
To cite this abstract in AMA style:
Webers C, Nezam El-Din R, Been M, Vonkeman H, van Tubergen A. Drivers of Treatment Intensification in Patients with Axial Spondyloarthritis and High Disease Activity: Results from a Clinical Practice Registry [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/drivers-of-treatment-intensification-in-patients-with-axial-spondyloarthritis-and-high-disease-activity-results-from-a-clinical-practice-registry/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/drivers-of-treatment-intensification-in-patients-with-axial-spondyloarthritis-and-high-disease-activity-results-from-a-clinical-practice-registry/