Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The number of clinical spondyloarthritis (SpA)-features plays an important role in the Assessment of SpondyloArthritis international Society (ASAS) modified Berlin algorithm for the diagnostic work-up of patients with a suspicion of axial SpA (axSpA). Therefore, we investigated whether all patients with short duration chronic back pain (CBP) and multiple SpA-features are always diagnosed as axSpA by rheumatologists and to describe the features of these patients.
Methods: The SPondyloArthritis Caught Early (SPACE)-cohort includes CBP patients ( ≥ 3 months, ≤ 2 years, onset < 45 years) from various rheumatology centers. Following a fixed protocol all patients underwent a full diagnostic work-up consisting of performance of MRI and radiographs of sacroiliac joints, acute phase reactants, HLA-B27, and assessment of other SpA-features (inflammatory back pain (IBP), good response to NSAIDs, family history for SpA, peripheral arthritis, dactylitis, enthesitis, uveitis, inflammatory bowel disease (IBD), and psoriasis). Each center interpreted the MRI-SI and X-SI on presence of sacroiliitis (yes/no) using global assessment as part of routine clinical practice. Total number of SpA-features was calculated after medical history taking, physical examination and measurement of acute phase reactants, excluding sacroiliac imaging and HLA-B27 status. The treating rheumatologist provided clinical diagnosis of patients and the ASAS-criteria for axSpA were used for classification.
Results: A total of 500 baseline patients were analysed in this study: 159 (31.8%) patients had ≤1 SpA-feature, 143 (28.6%) patients had 2 SpA-features, 79 (15.8%) patients had 3 SpA-features, and 119/500 (23.8%) patients had ≥4 SpA-features (Table 1). IBP, good response to NSAIDs, and positive family history for SpA were most common in all subgroups (≤1 feature: 27.0%, 8.2%, and 16.4%; 2 features: 72.0%, 35.0%, 39.9%; 3 features: 89.9%, 59.5%, 54.4%; ≥4 features: 94.1%, 82.4%, 67.2% ). Of the patients with 2 and 3 SpA-features without radiographic sacroiliitis 20/127 (15.7%) and 9/74 (12.2%) did not have axSpA diagnosis despite being HLA-B27+. All patients with ≥4 SpA-features and radiographic sacroiliitis (n=28) were diagnosed with axSpA. In contrast to what would be expected by following the modified Berlin algorithm for patients with ≥4 SpA-features 18/91 patients (19.8%) with negative imaging, 4 of whom were HLA-B27+, were not diagnosed with axSpA. In the majority of patients there was concordance between fulfilment of the ASAS classification criteria and axSpA diagnosis, however 40 patients who met the criteria were not diagnosed with axSpA.
Conclusion: In this cohort of CBP patients neither the mere presence of numerous SpA-features nor fulfilment of the ASAS classification criteria did automatically lead to axSpA diagnosis. Positive imaging was the main driving factor to diagnosis of axSpA. 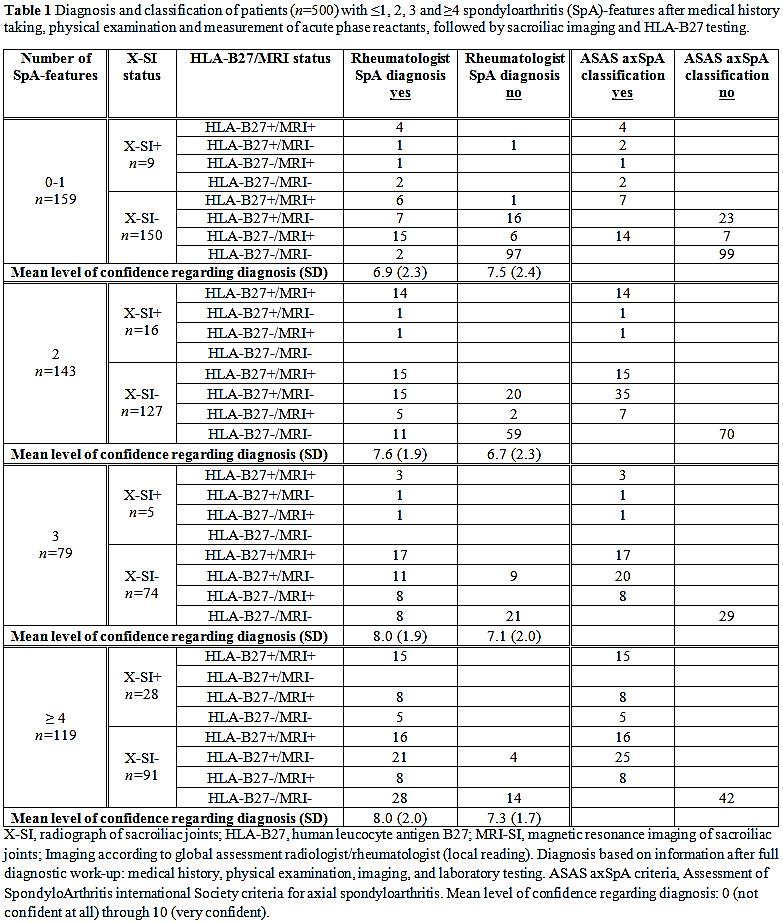
To cite this abstract in AMA style:
Ez-Zaitouni Z, Bakker P, van Lunteren M, Berg IJ, Landewé R, van Oosterhout M, Lorenzin M, van der Heijde D, van Gaalen F. Does the Presence of Multiple Spondyloarthritis-Features in Patients with Chronic Back Pain Always Lead to Diagnosis of Axial Spondyloarthritis? [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/does-the-presence-of-multiple-spondyloarthritis-features-in-patients-with-chronic-back-pain-always-lead-to-diagnosis-of-axial-spondyloarthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-the-presence-of-multiple-spondyloarthritis-features-in-patients-with-chronic-back-pain-always-lead-to-diagnosis-of-axial-spondyloarthritis/
