Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatic diseases are often at risk for opportunistic infections given the combination of disease manifestations and immunosuppressive treatment regimens, but the rates of Pneumocystis jiroveci pneumonia (PJP) are fairly low in this population. Prophylaxis against Pneumocystis jiroveci is often recommend for immunosuppressed transplant, leukemia and HIV patients, but there are no guidelines for patients with rheumatic diseases. The purpose of this study is to review the number of PJP cases at our institution in vasculitis patients and compare the rates of hospitalizations for other infections for patients receiving PJP prophylaxis to those who are not.
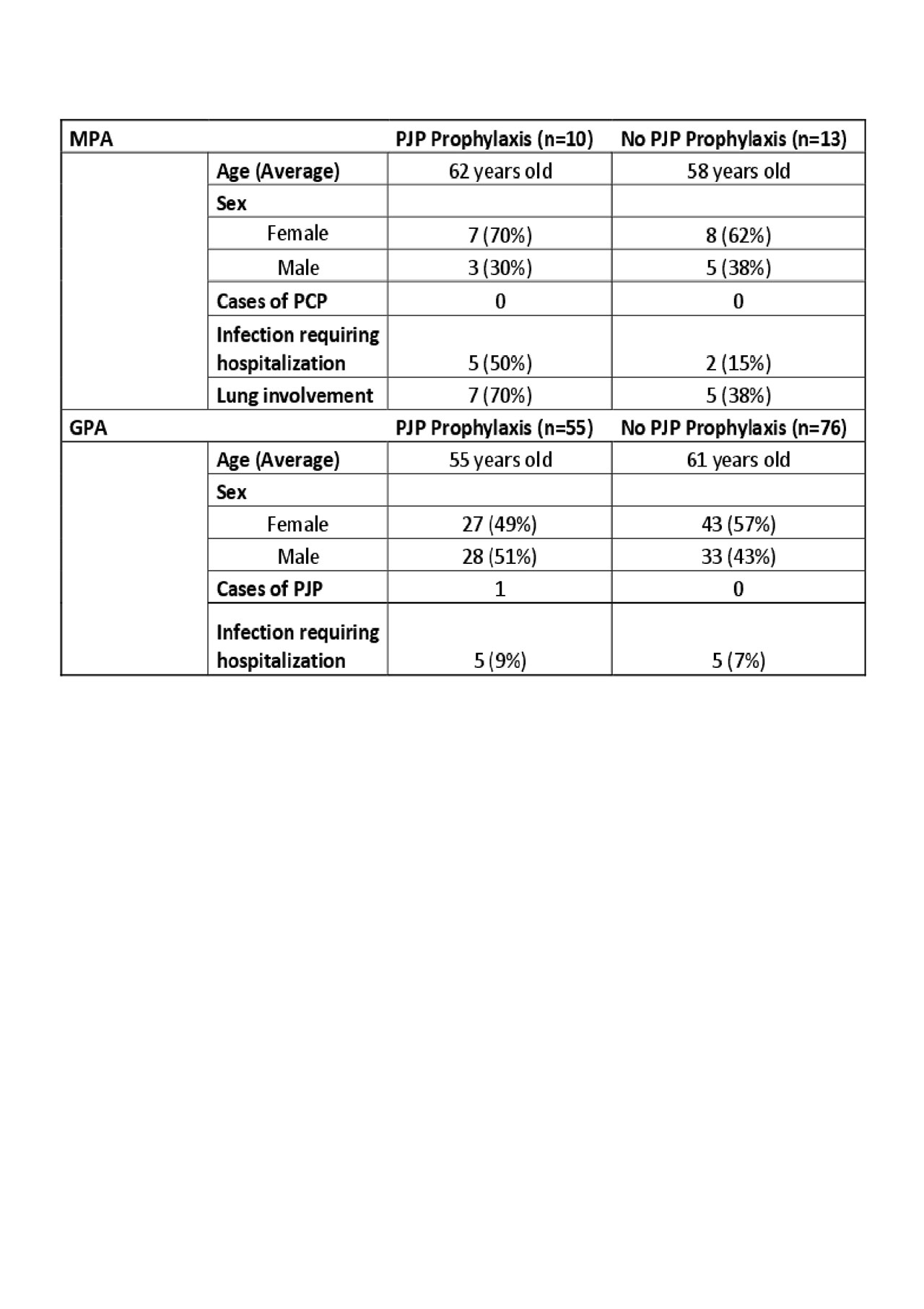
Methods: Using Epic’s Slicer Dicer tool, we selected microscopic polyangiitis (MPA) and granulomatosis with polyangiitis (GPA) patients over the past ten years who received care at our institution. Patients under 18 years-old, and patients without documented MPA or GPA were excluded. We then reviewed the electronic charts for these patients and recorded demographic information, PJP prophylaxis, hospitalizations at our institution for infections, disease and treatment information. Fisher’s exact test was used to compare rates of hospitalizations for infections for the PJP prophylaxis group vs. the non-prophylaxis group for MPA and GPA.
Results: Initially, 287 charts were reviewed and 154 met our inclusion criteria. Of all MPA and GPA charts reviewed, there was only one reported case of PJP listed in the past medical history of a GPA patient’s chart happened to be on PJP prophylaxis. This case was complicated by a history of renal transplant and it was unclear when PJP was contracted in relation to PJP prophylaxis timing. The PJP prophylaxis group for MPA and GPA together had more cases of hospitalizations due to infections. The majority of these infections were viral (influenza, CMV) and skin-related (abscesses and cellulitis). The p-value for GPA patients for infection hospitalizations between prophylaxis and non-prophylaxis groups was 0.7415 and was 0.1688 for MPA patients, neither of which were statistically significant.
Conclusion: The rate of PJP in our vasculitis population is low, as suggested by prior literature. Our results do not indicate that PJP prophylaxis decreases hospitalizations for infections in MPA or GPA patients, although our results likely underestimate the number of hospitalizations, since we were unable to include hospitalizations at other institutions. The next steps of this study will be to evaluate other diseases including EGPA, PM/DM, SLE, CTD-ILD for rates of PJP and hospitalizations for other infections.
To cite this abstract in AMA style:
Patel V, Trotter K. Does Pneumocystis Jiroveci Pneumonia (PJP) Prophylaxis Prevent Hospitalizations for Other Infections in Vasculitis Patients? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/does-pneumocystis-jiroveci-pneumonia-pjp-prophylaxis-prevent-hospitalizations-for-other-infections-in-vasculitis-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-pneumocystis-jiroveci-pneumonia-pjp-prophylaxis-prevent-hospitalizations-for-other-infections-in-vasculitis-patients/